
Report to Congress
Annual Report
on Self-Insured Group Health Plans
Martin J. Walsh
Secretary of Labor
March 2023
U.S. Department of Labor
2
Table of Contents
Executive Summary ......................................................................... 3
Introduction ...................................................................................... 6
Section I. Required Form 5500 Group Health Plan Data ................ 8
Section II. Additional Analysis of Financial Information on
Employers Sponsoring Self-Insured, Mixed-Insured, and Fully
Insured Group Health Plans ........................................................... 17
Section III. Conclusion .................................................................. 19
3
Annual Report to Congress on
Self-Insured Group Health Plans
Executive Summary
The Patient Protection and Affordable Care Act0F
1
requires the Secretary of Labor to provide
Congress with an annual report containing general information on self-insured employee
health benefit plans and financial information of employers that sponsor such plans. The
report must use data from the Annual Return/Report of Employee Benefit Plan (Form
5500), which many self-insured health plans must file annually with the Department of
Labor. The first report was provided to Congress in March 2011.1F
2
Along with this report, the Department is submitting two detailed appendices:
• Appendix A, Group Health Plans Report: Abstract of 2020 Form 5500 Annual
Reports Reflecting Statistical Year Filings, provides detailed statistics describing
group health plans that file a Form 5500.2F
3
• Appendix B, Self-Insured Health Benefit Plans 2023: Based on Filings through
Statistical Year 2020, explores statistical issues associated with Form 5500 health
plan data and analyzes available data on the financial status of employers that
sponsored group health plans and filed the Form 5500.3F
4
This report presents data on health benefit plans’ Form 5500 filings covering private-sector
employees for statistical year 2020, the latest year for which complete data are available.
Approximately 74,100 group health plans filed a Form 5500 for 2020, an increase of nearly
13 percent from 2019. Of those plans, about 37,900 were self-insured and 4,400 mixed
self-insurance with insurance (“mixed-insured”). Self-insured plans covered nearly 35
million participants and held more than $112 billion in assets, while mixed-insured plans
covered roughly 29 million participants and held $157 billion in assets.
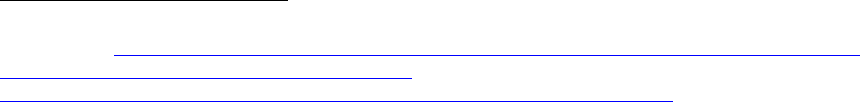
Table 1 summarizes aggregate statistics on plan counts, participants, and assets for self-
insured and mixed-insured group health plans that filed a Form 5500 for statistical years
2019 and 2020.
1
P.L. 111–148 (Mar. 23, 2010).
2
Available at https://www.dol.gov/sites/default/files/ebsa/researchers/statistics/retirement-bulletins/annual-
report-on-self-insured-group-health-plans-2011.pdf. The 2012–2022 reports are also available online at
https://www.dol.gov/agencies/ebsa/about-ebsa/our-activities/resource-center/reports. However, due to
changes to the algorithm and methodology beginning with the 2013 report, the reports are not comparable
over time.
3
This work was conducted for the Department by the Actuarial Research Corporation (ARC) under
contract number 1605DC-19-F-00326.
4
This work was conducted for the Department by Advanced Analytical Consulting Group (AACG) under
contract number 1605DC-19-C-0049.
4
Table 1. Group Health Plans That Filed Form 5500, Statistical Years 2019 and 2020*
Plan Type
2019
2020
Self-
Insured
Plans
Mixed-
Insured Plans
Self-
Insured
Plans
Mixed-
Insured Plans
All Plans 30,200 4,200 37,900 4,400
Participants 36 million 28 million 35 million 29 million
Active Participants† 32 million 25 million 31 million 25 million
Large Plans‡ Not Holding
Assets in Trusts
18,700 3,300 19,200 3,500
Participants
24 million
20 million
23 million
21 million
Active Participants
22 million
19 million
22 million
19 million
All Plans Holding Assets in
Trust
11,500 900 18,800 900
Participants 12 million 8 million 12 million 8 million
Active Participants 10 million 6 million 9 million 6 million
Assets $102 billion $145 billion $112 billion $157 billion
Contributions $63 billion $76 billion $61 billion $74 billion
Benefits $60 billion $77 billion $58 billion $74 billion
NOTES: All figures in this table have been rounded.
* The Department defines a “statistical year” Form 5500 filing population as all Form 5500 employee
benefit plan filings with a plan year ending date between January 1 and December 31 of a given year.
† See https://www.dol.gov/sites/dolgov/files/ebsa/employers-and-advisers/plan-administration-and-
compliance/reporting-and-filing/form-5500/2020-instructions.pdf.
‡ Plans with at least 100 participants.
SOURCE: 2019 and 2020 Form 5500 filings.
Sponsors of self-insured plans pay covered health expenses directly (either from their
general assets or from a trust), as the plans incur claims. Sponsors of fully insured plans
generally pay premiums to insurers that assume the responsibility of paying claims.
Sponsors of mixed-insured plans retain claims-paying responsibility for a subset of the
benefits but transfer the risk for the remaining benefits to insurers, therefore financing
benefits using a mixture of self-insurance and insurance. Self-insurance is more common
among larger group health plan sponsors, in part because the health expenses of larger
group health plans are more predictable and, therefore, larger plan sponsors face less risk.
Self-insured and fully insured group health plans are governed by somewhat different rules.
For example, state insurance laws generally do not apply to self-insured, ERISA-covered
health plans. Likewise, some Affordable Care Act provisions apply to group health
insurance but not to self-insured plans.
Generally, health benefit plans covering private-sector employees must file a Form 5500 if
they have 100 or more participants. Regardless of size, plans must file a Form 5500 if they
hold assets in trust or are identified as a Multiple Employer Welfare Arrangement (MEWA)
or certain Entities Claiming Exception (ECE).
5
Most small (typically fewer than 100 participants), ERISA-covered group health plans do
not hold assets in trust and, therefore, are not required to file a Form 5500. As a result, a
large majority of small health benefit plans – including a significant but unknown number
of small, self-insured plans – are not included in this report.
The Department estimates that there were about 2.5 million ERISA-covered group health
plans covering approximately 133 million participants and beneficiaries in 2020.4F
5
Only
about 74,100 plans covering 78 million participants filed a 2020 Form 5500.5F
6
Of those
group health plans, about 36,100 filed at least one Schedule A (Insurance Information) for
a group insurance policy covering health benefits6F
7
and roughly 20,400 plans reported
holding assets and filed a Schedule H (Financial Information) or Schedule I (Financial
Information–Small Plan).7F
8
The Form 5500 does not collect data on plan sponsors’ finances.8F
9
However, financial data
for a subset of sponsoring employers that issue publicly traded equity or debt are available
from other sources.9F
10
The financial strength of these plan sponsors varies considerably.
Similar variation is found among employers that sponsor self-insured plans, mixed-insured
plans, and fully insured plans.
5
EBSA health plan estimates are based on the 2021 Medical Expenditure Panel Survey, Insurance
Component (MEPS-IC) and the 2019 County Business Patterns from the Census Bureau. Counts of
participants and beneficiaries for calendar year 2020 are from Table 1A of the Health Insurance Coverage
Bulletin: Abstract for the March 2021 Annual Social and Economic Supplement to the Current Population
Survey, https://www.dol.gov/sites/dolgov/files/EBSA/researchers/data/health-and-welfare/health-
insurance-coverage-bulletin-2021.pdf.
6
See Appendix A, Table A1.
7
See Appendix A, Table B1.
8
Statistics from Appendix A, Table A2 and ad-hoc tabulations produced by Actuarial Research
Corporation (ARC)
9
For multiemployer plans in particular, the plan sponsor is the association, committee, joint board of
trustees, or other similar group of representatives of the parties who establish or maintain the plan and
generally does not have finances separate from the plan.
10
The analysis in this report relies on Bloomberg data, which culls Form 10-K filings and other sources to
collect data on companies with public financial statements, and generally includes companies with publicly
traded stock or bonds.
6
Introduction
Section 1253 of the Patient Protection and Affordable Care Act (Affordable Care Act) (P.L.
111–148) requires the Secretary to prepare an aggregate annual report that includes certain
general information on self-insured group health plans using data collected from the
Annual Return/Report of Employee Benefit Plan (Form 5500),10F
11
as well as certain data
from financial filings of self-insured employers.
Sponsors of self-insured plans generally pay their plans’ covered health expenses directly,
as the plans incur claims. In contrast, sponsors of fully insured plans typically pay
premiums to insurers, which, in turn, assume the responsibility of paying claims. Sponsors
of mixed-insured plans retain this responsibility for a subset of benefits, but transfer the
risk for the remaining benefits to health insurers—that is, they finance benefits using a
mixture of self-insurance and insurance.
There are key qualitative differences between the three categories of plans: self-insured
plans, fully insured plans, and mixed-insured plans.11F
12
Currently, the Form 5500 does not
explicitly disclose whether a health plan is self-insured, so the Department created an
11
The following welfare plans, including group health plans, are not required to file a Form 5500, due to
statutory exemptions from ERISA or regulatory exemptions:
• welfare plans (other than plans required to file the Form M-1) with fewer than 100 participants as
of the beginning of the plan year (small plans) that are unfunded, fully insured, or a combination
of insured and unfunded;
• welfare plans maintained outside the United States that serve mostly nonresident aliens;
• governmental plans;
• unfunded or insured welfare plans maintained for a select group of management or highly
compensated employees only;
• plans maintained only to comply with workers’ compensation, unemployment compensation, or
disability insurance laws;
• welfare benefit plans that participate in a group insurance arrangement that files a Form 5500 on
behalf of the plan;
• apprenticeship or training plans meeting certain conditions;
• certain dues financed unfunded welfare benefit plans where certain reports are filed under the
Labor-Management Reporting and Disclosure Act;
• church plans; and
• welfare benefit plans maintained solely for the owner and/or spouse who wholly own a trade or
business or the partners and/or spouses of partners in a partnership.
A small plan that (1) receives employee (or former employee) contributions during the plan year and does
not use the contributions to pay insurance premiums or (2) uses a trust or separately maintained fund to
hold plan assets or act as a conduit for the transfer of plan assets during the year is generally required to
file. However, a small plan with employee contributions that are used to pay benefits instead of insurance
premiums and is associated with a cafeteria plan under Internal Revenue Code section 125 may be treated
as an unfunded welfare plan for annual reporting purposes if it meets certain Department requirements.
(See 29 C.F.R. 2520.104-1 et seq.) In addition, plans that are MEWAs required to file the Form M-1 must
file the Form 5500, regardless of plan size. See https://www.dol.gov/sites/dolgov/files/ebsa/employers-and-
advisers/plan-administration-and-compliance/reporting-and-filing/forms/m1-2020.pdf.
12
Annual Report on Self-Insured Group Health Plans, Section III, What is a Self-Insured Group Health
Plan? (U.S. Department of Labor, March 2011). See
https://www.dol.gov/sites/dolgov/files/EBSA/researchers/statistics/retirement-bulletins/annual-report-on-
self-insured-group-health-plans-2011.pdf.

7
algorithm using filing characteristics to sort plans as self-insured, fully insured, or mixed-
insured.
The methodologies for determining the plan universe for analysis and for determining
group health plans’ funding mechanism have periodically evolved since the March 2013
report. The Department has used its current methodologies to incorporate previous years’
data into this report to facilitate comparisons over time.12F
13
However, because of these
methodology changes, one cannot identify trends over time merely by directly comparing
the numbers in the reports.
In some instances, group health benefits are offered through a plan that provides coverage
to the employees of two or more employers (and is not a collectively bargained
arrangement). Such a plan generally constitutes a MEWA under ERISA and is required to
file a Form 5500 regardless of size or holding of assets. The Department classifies and
reports plans according to their sponsor type: single-employer plans, multiemployer plans,
and multiple employer plans.13F
14
13
Subject to the following criteria, the analysis for this report is based on health benefit plans that filed a
Form 5500 or Form 5500-SF.
1. Test filings, direct filing entity filings (including group insurance arrangements [GIAs], which can
only file on behalf of participating plans if it is fully insured and uses a trust), duplicative filings,
and filings for “one-participant” retirement plans with health plan features have been removed
from the raw data set prior to analysis. Because some GIAs provide fully insured group health
benefits, the number of participants receiving fully insured group health benefits that are covered
by Title I of ERISA and reported on the Form 5500 may be understated. Information on the 37
Health GIAs that filed in 2020 is found in Appendix A of this report.
2. “Voluntary” filers (i.e., those that appear to meet the exception from the requirement to file based
on the information provided, but still filed) have been excluded from the analysis. Filers with
fewer than 100 beginning-of-year (BOY) participants and no assets held were dropped from the
universe, including those with the following fields equal to zero or left blank on their Form 5500-
SF or Schedule I or H:
a. Beginning/End-of-Year Assets, Liabilities, and Net Assets
b. Income, Expenses, and Net Income
3. For Form 5500-SF filers with fewer than 100 BOY participants and showing financial
information, we have assumed that it was an appropriate filing and that the plan must be self-
insured.
4. Terminating trusts and plans that file zero end-of-year (EOY) participants have been included.
5. For plans with missing EOY participants that are nonterminating, BOY participants have served as
a proxy for EOY total and active participants.
14
Beginning with the Statistical Year 2017 filings, any plan that self-identifies as a multiple employer plan
is classified as a multiple employer plan. In addition, plans that identify as multiemployer plans are
reclassified as multiple employer plans if they report a business code of offices of physicians or dentists,
real estate, or legal services. Of the 74,100 group health plans in this year’s report, 841 were classified as
multiple employer plans. Of those, 258 were self-insured and 68 were mixed-insured.

8
Section I. Required Form 5500 Group Health Plan Data
Section 1253 of the Affordable Care Act requires the Department to submit information
on several data items from the Form 5500:
a) “general information on self-insured group health plans (including plan type,
number of participants, benefits offered, funding arrangements, and benefit
arrangements)”
b) “data from the financial filings of self-insured employers (including information
on assets, liabilities, contributions, investments, and expenses).”
The Form 5500 data presented below in response to these requirements should be
carefully interpreted for several reasons.14 F
15
• The Department has information for these data items only for those plans that are
required to file a Form 5500. Generally, group health plans covering private-
sector employees must file a Form 5500 only if they cover 100 or more
participants, hold assets in trust, or constitute a plan MEWA. Governmental and
church plans, regardless of size, are not required to file a Form 5500. Therefore,
information concerning such plans is not available in the Form 5500 data and is
not included in the statistics provided in this report.
• Self-insured welfare benefit plans, including group health plans, are generally
required to file financial information only about assets they hold in trust. Thus,
the aggregate financial statistics provided in this report are understated insofar as
they do not include health benefits paid directly from plan sponsors’ general
assets. Of the self-insured plans that filed a Form 5500 in 2020, 51 percent did not
hold assets in trust, and thus did not report financial information.
• In cases where a single plan provides several different types of welfare benefits,
health benefits provided under the plan may be reported together with certain
other welfare benefits, such as disability or life insurance benefits, on a single
Form 5500. This can make it difficult to determine how the different benefits are
financed and whether the group health component of the plan is self-insured or
fully insured.15F
16
As a result, the estimates presented here are subject to substantial
uncertainty.
15
See the section titled “The Definition of Self-Insurance” in Appendix B for a detailed description of the
Department’s method for estimating whether group health plans are self-insured, fully insured, or “mixed-
insured,” based on the Form 5500 data.
16
See report, Strengths and Limitations of Form 5500 Filings for Determining the Funding Mechanism of
Employer-Provided Group Health Plans, at
https://www.dol.gov/sites/default/files/ebsa/researchers/analysis/health-and-welfare/strengths-and-
9
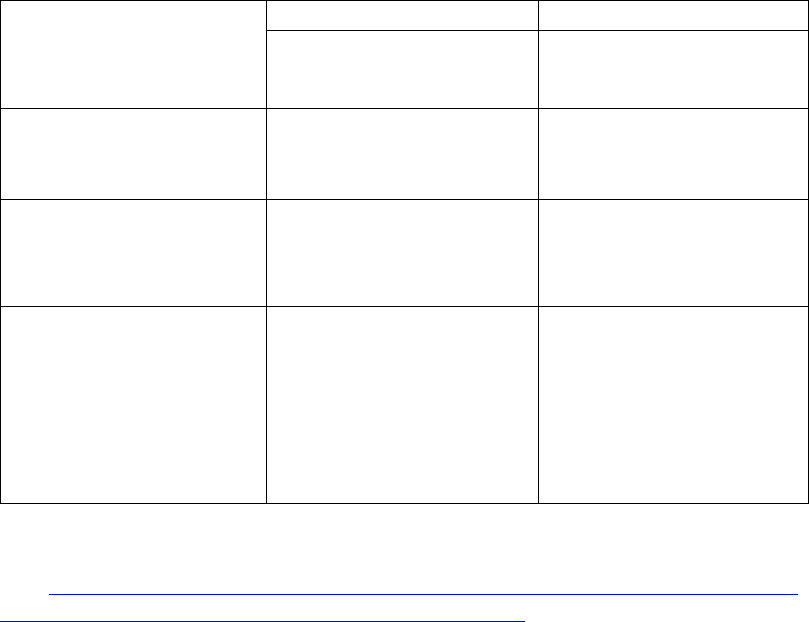
Table 2. Form 5500 Group Health Plans Summary Information, 2020 Statistical Year
Filings
Plan Type All Plans
Self-Insured
Plans
Mixed-
Insured
Plans
Fully Insured
Plans*
All Plans
74,100
37,900
4,400
31,700
Participants
78 million
35 million
29 million
14 million
Active Participants
70 million
31 million
25 million
13 million
Large Plans Not Holding Assets
in Trusts
53,700 19,200 3,500 31,000
Participants
56 million
23 million 21 million 12 million
Active Participants
53 million
22 million 19 million 12 million
All Plans Holding Assets in Trust
20,400
18,800
900
700
Participants
22 million
12 million
8 million
2 million
Active Participants
17 million
9 million
6 million
2 million
Assets
$283 billion
$112 billion
$157 billion
$14 billion
Contributions
$150 billion
$61 billion
$74 billion
$15 billion
Benefits
$147 billion
$58 billion
$74 billion
$15 billion
NOTES: All figures in the table have been rounded. Totals may not equal the sum of the components due
to rounding.
* Plans that report benefit payments are classified as fully insured only if other information on the Form
5500 filing suggests that these payments were made to insurance companies for the provision of benefits
and not made directly to participants.
SOURCE: 2020 Form 5500 filings.
Plan Type by Funding Mechanism
Funding mechanism refers to the method by which a health plan finances its benefits.
Plan sponsors may choose to pay for health services directly through general assets of the
sponsor, with plan assets, by purchasing insurance to cover benefit obligations, or some
combination. For purposes of this report, the Department classifies those arrangements as
“self-insured,” “fully insured,” or “mixed-insured” respectively.
Of the self-insured group health plans:
• about 36,700 were sponsored by single employers,
• about 1,000 were multiemployer plans, and
• fewer than 300 were multiple employer plans.16F
17
limitations-of-form-5500-filings-for-determining-the-funding-mechanism-of-employer-provided-group-
health-plans.pdf for a discussion of the sensitivity of plans’ funding categorizations. This work was
conducted for the Department by Deloitte Financial Advisory Services LLP under task order number
DOLB109330993.
17
For certain Form 5500 reporting purposes, a “controlled group” or affiliated service group under Code
section 414(b), (c), or (m) is generally considered a single employer.
10
Of the mixed-insured group health plans:
• about 4,100 were sponsored by single employers,
• about 300 were multiemployer plans, and
• fewer than 70 were multiple employer plans.17F
18
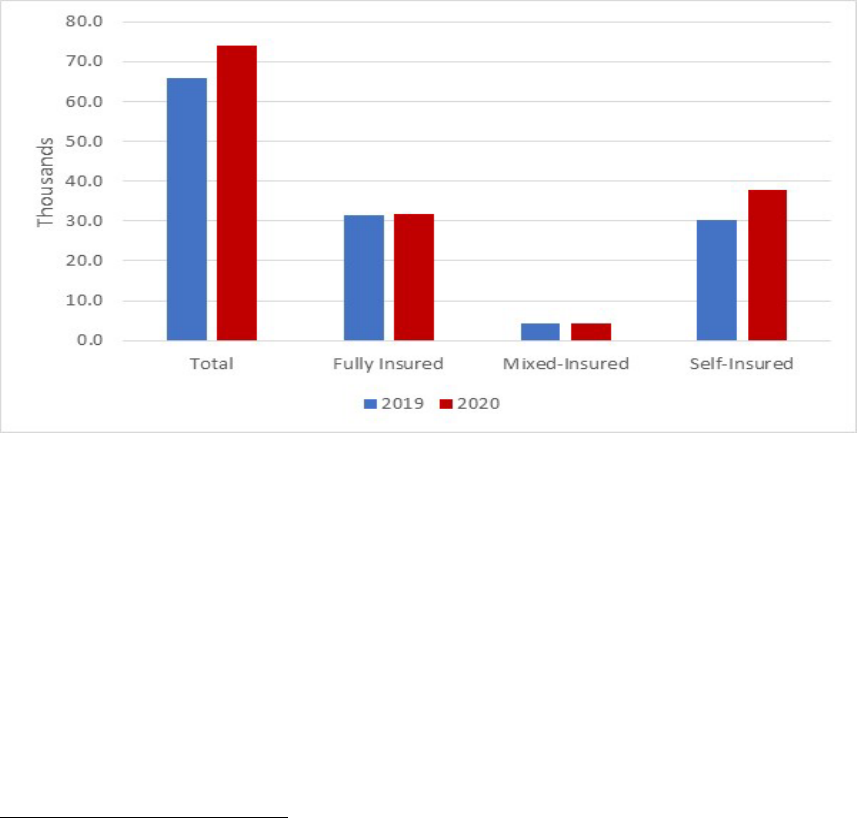
The number of group health plans that filed a Form 5500 increased by 13 percent
between 2019 and 2020. While all types of plans increased, the number of self-insured
plans grew most significantly, at nearly 26 percent.18F
19
This growth was largely driven by a
78 percent increase in filings of small, self-insured plans.19F
20
Figure 1. Group Health Plans that Filed a Form 5500, 2019-2020
SOURCE: Appendix B, Tables 7 and 18.
Number of Participants
The approximately 37,900 self-insured group health plans covered 35 million
participants, 31 million of whom were active participants. The 4,400 mixed-insured
group health plans covered approximately 29 million participants, 25 million of whom
were active participants.2 0F
21
Plans covering a larger number of participants are more likely to be self-insured than
plans with fewer participants. While 55 percent of large plans were fully insured, only 18
percent of participants were covered by large fully insured plans.2 1F
22
18
See Appendix A, Table A2.
19
See Appendix B, Table 2 and Table 18.
20
See Appendix B, Table 2.
21
See Appendix A, Table A1.
22
See Appendix B, Table 5.
11
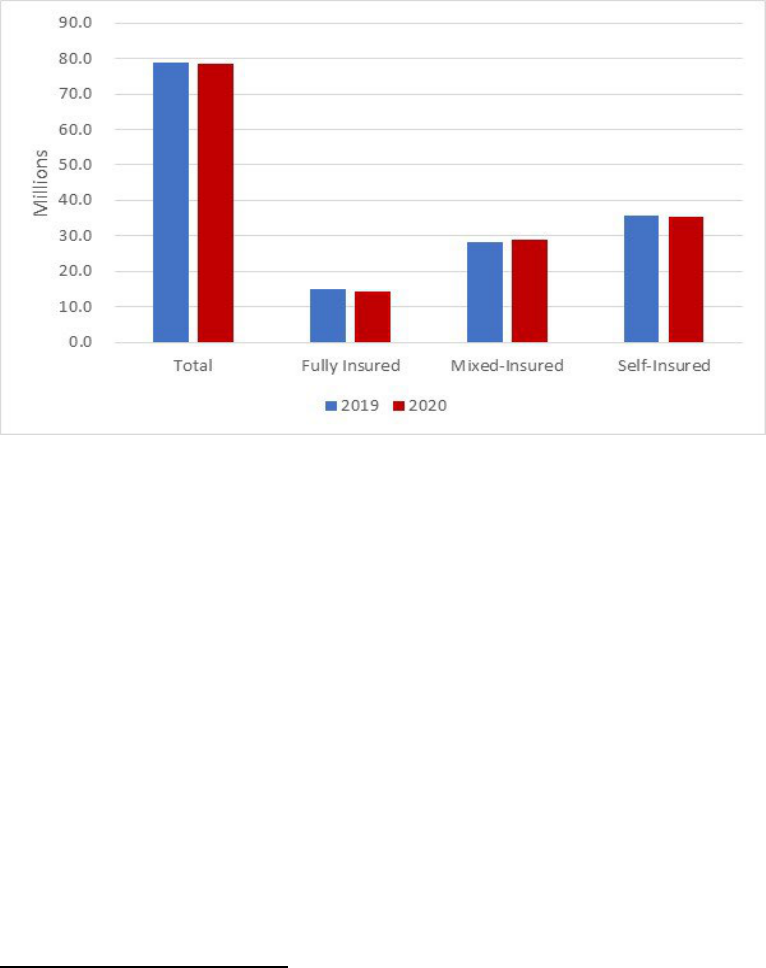
Although the number of plans increased by nearly 13 percent between 2019 and 2020,
participant growth declined by almost 1 percent. However, the distribution of participants
by funding type remained largely unchanged.22F
23
Figure 2. Participants in Group Health Plans that Filed a Form 5500, 2019-2020
SOURCE: Appendix B, Tables 7 and 18.
New Plans
New health plans are defined as health plans that checked the “first return/report filed for
the plan” box on their Form 5500 filing.23F
24
Of the roughly 10,500 new group health plans,
75 percent were small plans.
While new large plans tended to be fully insured (73 percent), new, small plans were
overwhelmingly self-insured (99 percent), primarily due to an influx of filings by small,
self-insured plans that participate in non-plan MEWAs.2 4F
25
Participants in new, large plans were split among funding types:
• 45 percent were covered by self-insured group health plans,
• 17 percent by mixed-insured group health plans, and
23
See Appendix B, Table 7 and Table 18.
24
Beginning with the 2013 Self-Insured Report to Congress, plans were identified as “new” if they checked
the “first return/report filed for the plan” box on their Form 5500. Prior to this, plans were identified as
“new” if they could not be matched to a plan filing in a prior year, going back to 2001, regardless of
whether they reported the filing as their first filing. Consequently, the number of “new” plans in the current
Self-Insured Report to Congress is not directly comparable to the numbers reported in years prior to 2013.
25
See Appendix B, Table 8 and Table 21.

12
• 38 percent by fully insured plans.25F
26
However, 93 percent of participants in new, small plans were covered by self-insured
plans.26F
27
Benefits Offered
About 17,800 self-insured group health plans offered only health benefits, and 20,200
offered health and other benefits.2 7F
28
More than 250 mixed-insured group health plans offered only health benefits, and 4,100
offered health and other benefits.2 8F
29
Funding and Benefit Arrangements
Funding Arrangements
A funding arrangement is the method by which the plan receives, holds, invests, and
transmits assets that have not yet been used to provide benefits.
Among the self-insured group health plans, approximately:
• 1,600 indicated a trust-only funding arrangement,
• 1,500 indicated a funding arrangement of trust with insurance,
• 3,900 indicated funding from the general assets of the sponsor only,
• 15,000 indicated funding from the general assets of the sponsor combined with
insurance,29F
30
and
26
See Appendix B, Table 8.
27
See Appendix B, Table 21.
28
Note that a health-only plan does not imply that the sponsor only offers health benefits. For example, the
sponsor could simultaneously offer a separate life insurance plan for which a separate Form 5500 filing
exists. This report does not include information on welfare plans that do not provide health benefits.
29
See Appendix A, Table A1. Totals do not sum due to rounding.
30
The majority of plans indicating a funding arrangement of general assets combined with insurance filed a
Schedule A (Insurance) for a nongroup health benefit. Alternatively, they were self-insured plans with stop-
loss coverage or plans that check box 9a on the Form 5500 indicating insurance, but did not file a Schedule
A.

13
• 16,000 indicated insurance alone,3 0F
31
some other combination of funding
arrangements, or did not report any arrangement.31F
32
Among the mixed-insured group health plans:
• 200 indicated a trust-only funding arrangement,
• 500 indicated a funding arrangement of trust with insurance,
• 3,400 indicated a funding arrangement of general assets of the sponsor combined
with insurance,32F
33
and
• the remaining indicated insurance alone or some other combination of funding
arrangements.3 3F
34
Benefit Arrangements
A benefit arrangement is the method by which the plan provides benefits to participants.
Among the self-insured group health plans, approximately:
• 1,000 indicated a benefit arrangement of a trust only,
• 2,100 indicated a benefit arrangement of trust with insurance,
• 3,500 indicated a benefit arrangement of general assets of the sponsor only,
• 15,300 indicated a benefit arrangement of general assets of the sponsor combined
with insurance,34F
35
and
• 16,100 indicated insurance alone, some other combination of benefit
arrangements, or did not report any arrangement.
Among the mixed-insured group health plans, approximately:
• 700 indicated a benefit arrangement of trust with insurance,
• 3,500 indicated a benefit arrangement of general assets of the sponsor combined
with insurance, and
31
Totals do not sum due to rounding. There were 485 of these plans that indicated “insurance alone” as a
funding arrangement in their filing but were characterized as “self-insured” for this report. However, these
plans also indicated stop-loss insurance, per-capita insurance premiums consistent with an administrative
services only (ASO) contract, attached a Schedule H or I that suggested a trust and self-insurance, or a
combination. As a result, the Department assigned a funding mechanism of “self-insured” despite the plan
indicating a funding arrangement of “insurance alone” for purposes of this report.
32
See Appendix A, Table A7.
33
See Appendix A, Table A7. The 233 plans that were identified as mixed-insured and indicated a funding
arrangement of a trust only also filed a Schedule A (Insurance) and reported a health insurance contract.
Plans are deemed mixed-insured if the trust payments and the reported premium payments are more than 20
percent apart, if the percentage of participants covered by reported health insurance contracts is less than
50, or if the trust payments made directly to participants were substantial. (See Appendix B, pages 13–20)
34
See Appendix A, Table A7.
35
The self-insured plans that listed a benefit arrangement of general assets of the sponsor combined with
insurance may have filed a Schedule A for a nongroup health benefit or stop-loss coverage, or they may
have checked box 9a on the Form 5500 indicating insurance but did not file a Schedule A.

14
• the remaining indicated insurance or trust alone, or some other combination of
benefit arrangements.35F
36
Stop-Loss Insurance
Self-insured plans may purchase stop-loss insurance to mitigate the risk of unexpectedly
large medical claims. Stop-loss insurance contracts protect against claims that are
catastrophic or unpredictable by covering claims costs that exceed a set amount for either
a single enrollee or for aggregate claims over a determined period.
If a sponsor purchases stop-loss insurance for its own benefit, the stop-loss insurance is
generally not required to be reported on Schedule A (Insurance). Accordingly, the
existence of stop-loss insurance as part of the sponsor’s arrangement for the plan is
understated in Form 5500 filings, especially for those plans that do not use a trust.
From 2011 to 2020, the percentage of large group health plans that reported having stop-
loss insurance gradually declined, from approximately 27 percent to 22 percent for self-
insured plans and from 21 percent to 17 percent for large mixed-insured plans.36F
37
It was markedly different for small group health plans. The percentage of self-insured
small plans that reported having stop-loss insurance increased from 13 percent in 2011 to
42 percent in 2020, though the percentage of mixed-insured plans that reported having
stop-loss insurance decreased from 48 percent to 33 percent.37F
38
Plan Assets and Liabilities of Plans That Financed Benefits through Trusts
Roughly 18,800 self-insured group health plans operated trusts. These plans reported
approximately $112 billion in assets (9 percent more than in 2019) and $11 billion in
liabilities (a half percent decrease compared with 2019).
About 900 mixed-insured group health plans financed benefits through trusts. These
plans reported nearly $157 billion in assets (8 percent more than in 2019) and $19 billion
in liabilities (16 percent more than in 2019).38F
39
36
See Appendix A, Table A7. Totals may not sum due to rounding.
37
See Appendix B, Table 12.
38
See Appendix B, Table 22.
39
See Appendix A, Table A2.

15
Contributions, Investments, and Expenses of Plans That Financed Benefits through
Trusts
Contributions & Benefit Payments
Self-insured group health plans that financed benefits through a trust received
approximately $61 billion in contributions and paid approximately $58 billion in benefit
payments. Of the amount paid:
• $47 billion was paid directly to participants or beneficiaries,
• $5 billion was paid to insurance carriers for the provision of benefits,39F
40
and
• $5 billion was reported as “other” and cannot be categorized.
Mixed-insured group health plans that financed benefits through a trust received
approximately $74 billion in contributions and paid approximately $74 billion in benefit
payments. Of the amount paid:
• $54 billion was paid directly to participants or beneficiaries,
• $18 billion was paid to insurance carriers for the provision of benefits, and
• $2 billion was reported as “other” and cannot be categorized.40F
41
Administrative Expenses
Self-insured group health plans reported paying about $4 billion in administrative
expenses, with approximately:
• $500 million in professional fees,
• $1.5 billion in contract administrator fees,
• $200 million in investment advisory and management fees, and
• $1.7 billion in other administrative expenses.
Mixed-insured group health plans reported paying about $4 billion in administrative
expenses, with approximately:
• $300 million reported as professional fees,
• $1.8 billion reported as contract administrator fees,
• $400 million reported as investment advisory and management fees, and
• $1.4 billion reflected as other administrative expenses.41 F
42
40
Plans that self-insure health benefits may make payments to insurance companies for administrative
services, stop-loss contracts, or insurance premiums for other types of benefits (such as dental or
disability).
41
See Appendix A, Tables A4 and A5.
42
Total for mixed-insured does not sum due to rounding. See Appendix A, Table A5.

16
Asset Holdings
The asset holdings reported by self-insured group health plans were composed of:
• 15 percent in cash and U.S. government securities,
• 21 percent in direct filing entities (DFEs),
• 27 percent in mutual funds (also known as registered investment companies),
• 9 percent in debt instruments, and
• 8 percent in stock.42F
43
The asset holdings reported by mixed-insured group health plans were composed of:
• 23 percent in cash and U.S. government securities,
• 11 percent in DFEs,
• 9 percent in mutual funds,
• 17 percent in debt instruments, and
• 10 percent in stock.43F
44
43
DFEs are pooled investment arrangements, including master trust investment accounts, insurance
company pooled separate accounts, bank common/collective trusts, other plan asset pooled investment
funds (103-12 investment entities), and group insurance arrangements (GIAs). A Form 5500 must be filed
for a master trust investment account. A Form 5500 is not required for the other entities, but for plans to get
reporting relief with respect to those entities, the entity must file a Form 5500. Each DFE lists the plans
whose assets it holds on Form 5500, Schedule D Part 2.
44
See Appendix A, Table A6.

17
Section II. Additional Analysis of Financial Information on
Employers Sponsoring Self-Insured, Mixed-Insured, and
Fully Insured Group Health Plans
Section 1253 of the Affordable Care Act requires this report to include data from the
financial filings of self-insured employers, including information on assets, liabilities,
contributions, investments, and expenses.
Data on the financial position of the plan sponsor or employer are not included in Form
5500 filings. In order to provide data on financial filings of self-insured employers, Form
5500 data were matched to Bloomberg financial data available for a select group of
companies with publicly traded equity or debt.44F
45
Analysis of financial measures –
including revenue, market capitalization, profit, and number of employees – shows that
companies offering self-insured or mixed-insured group health plans tend to be larger than
companies offering fully insured plans.45F
46
The results of matching the 2020 Form 5500 data to the Bloomberg financial data were
similar to the results for 2019. Approximately 3,400 Form 5500 filers, or 6 percent of large
plans in the 2020 Form 5500 health plan data, were matched to the Bloomberg data.
Because the Bloomberg data represents mostly large, publicly traded companies that are
based in the United States, the findings cannot be generalized and applied to smaller,
privately held companies or employers participating in multiemployer or multiple
employer plans.46F
47
Of the participants in matched plans, 88 percent were covered through
a plan with 5,000 or more participants.
Approximately 1,600 employers matched to a large, self-insured health plan. These plans
were sponsored by employers reporting a median employee count of 7,000, a median
revenue of approximately $2.5 billion, a median market capitalization of approximately
$4.4 billion, and a median profit of approximately $86 million.
Approximately 900 employers matched to a large, mixed-insured health plan. These plans
were sponsored by employers reporting a median employee count of 13,000, a median
revenue of approximately $4.7 billion, a median market capitalization of approximately
$8.3 billion, and a median profit of approximately $170 million.47F
48
45
Appendix B outlines this analysis. Bloomberg is a provider of financial and other data for private and
public companies in the United States. The data include company characteristics, financial health, and
financial size. Prior iterations of this report used corporate financial data from Capital IQ, which is very
similar to Bloomberg data.
46
See Appendix B, Table 14, for the distribution of the measures for each of the three categories of plans.
47
See Appendix B, Table 4. While this is a relatively small number, many companies that filed a Form
5500 are not represented in Bloomberg data because they may be exempt from publicly issuing financial
statements. Sponsors may be privately held, based overseas, or not-for-profit and without publicly issued
bonds; or the plan may be a multiemployer or multiple-employer plan.
48
See Appendix B, Table 14. Not all financial information for all employers was reported in the Bloomberg
data, so the number of observations used to calculate the reported medians varies significantly.

18
The financial health of the matched companies was measured using three financial metrics
and the distribution of their scores were reported by plan funding type.48F
49
Overall, the
results varied.
Employers sponsoring large, fully insured plans have more cash flow relative to total debt
than employers sponsoring mixed- or self-insured plans. As a result, a larger share of
employers sponsoring fully insured plans were in the top two categories of the cash/debt
measure than employers sponsoring either self-insured or mixed-insured plans. However,
a larger share of employers sponsoring fully insured plans had worse scores for operating
profit-to-debt ratio as well as the Altman Z-score, which is an index summarizing five
financial measures that predict bankruptcy risk, than self-insured or mixed-insured plans.
This variance makes it difficult to draw conclusions regarding the financial health of a
company and its choice of funding mechanism for its health plan, particularly as this
analysis is limited to large, publicly traded companies. It is noteworthy that, similar to prior
years, there was generally greater variation in the financial health of companies sponsoring
fully-insured plans than self- or mixed-insured plans.
Plans filing a Form 5500 can also be matched across years to determine what changes the
plan has undergone over time. From 2011 to 2020, 81 percent of plans, on average, were
matched to their previous years’ filing.49F
50
While plans may switch their funding mechanism
over time, less than 10 percent of large, established50F
51
plans do.51F
52
Established large plans
that do change their funding mechanism status continue to move away from being fully
insured. Large, fully insured plans are more likely to terminate.52F
53
The fact that large, fully insured plans are more likely to change their funding mechanism
or terminate than other large plans, coupled with the growth of new, self-insured plans –
which is driven by a large number of small plans that participate in a MEWA53F
54
– may
explain the increasing number of self-insured and mixed-insured plans as well as the
increased share of participants covered by self-insured and mixed-insured plans. New plans
are dominated by small, self-insured plans, and established plans tend to be larger than new
plans and, on net, move away from full insurance.54 F
55
49
See Appendix B, Figure 12.
50
See Appendix B, Table 3. The analysis of small plan behavior over time is limited, as small plans may
stop filing because their funding changed or because they terminated.
51
For this purpose, “established plans” are those that did not indicate being initial or final filings on their
Form 5500.
52
See Appendix B, Table 10.
53
See Appendix B, Table 11.
54
See Appendix B, Table 8 and Table 21.
55
See Appendix B, Table 11.
19
Section III. Conclusion
This Annual Report to Congress on Self-Insured Group Health Plans (March 2023)
provides the most detailed statistics currently available on self-insured group health plans
that filed a Form 5500 and on the sponsors of such plans that issue publicly traded equity
or debt. This report also documents the limited scope of such data and the complexities
involved in interpreting it.
The Department recognizes the importance of quality data. Accordingly, the Department
strives to further enhance this annual report and its underlying statistics to continue to
inform Congress on self-insured employee health benefit plans and financial information
regarding employers that sponsor such plans.
