Welcome to Alomere Health
It is our pleasure to serve you during your hospital stay.
Alomere Health provides a full multidisciplinary team to
help meet your needs. We all want to meet your
expectations with us.
We rely on our Alomere Team to help meet your needs.
Your team may include the following:
• Food and Nutrition Services
• Laboratory Staff
• Nursing Staff
• Pharmacy Staff
• Providers
• Radiology Staff
• Rehab Services
• Respiratory Therapy
• Social Workers
Be sure to communicate questions or concerns to any of
the team members.
111 - 17
th
Avenue East
Alexandria MN 56308
320.762.1511
For the most up to date patient
admission information please
visit:
alomerehealth.com/about/patient-
care-safety/
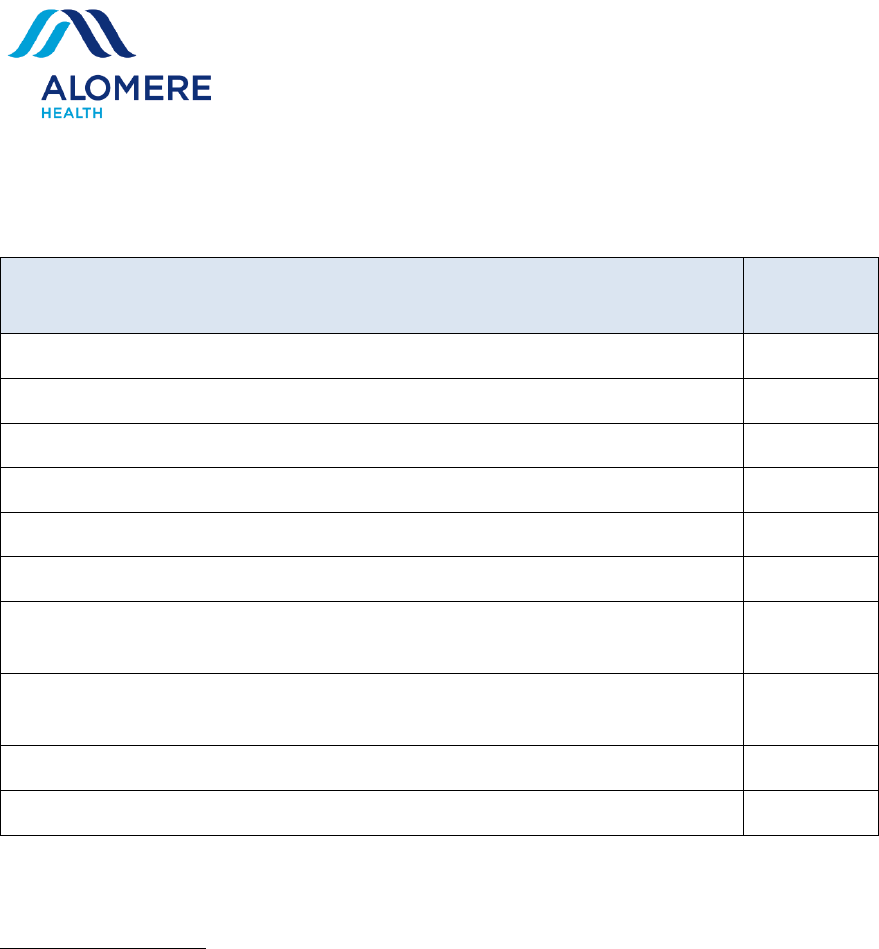
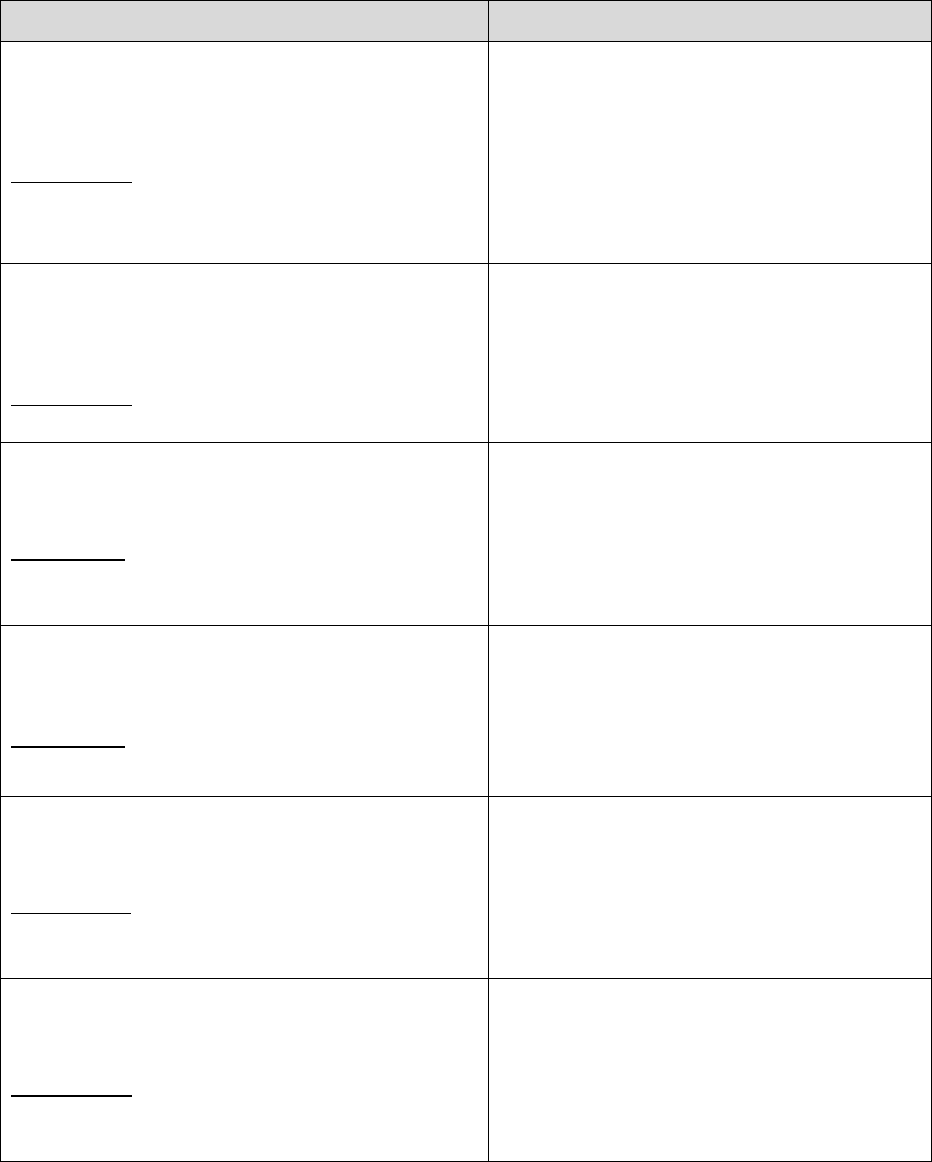
Table of Contents
Information
Page
Number
What You Should Know about Nursing Home Coverage
1
Outpatient/Observation Patient Status
2
Patient Rights
5
Grievance Process
11
Vulnerable Adults
12
Health Care Directives
14
Patient Safety (Safe Patient Handling, Prevention of: Blood Clots,
Skin Breakdown and Falls; What You Can Do to be Safe)
18
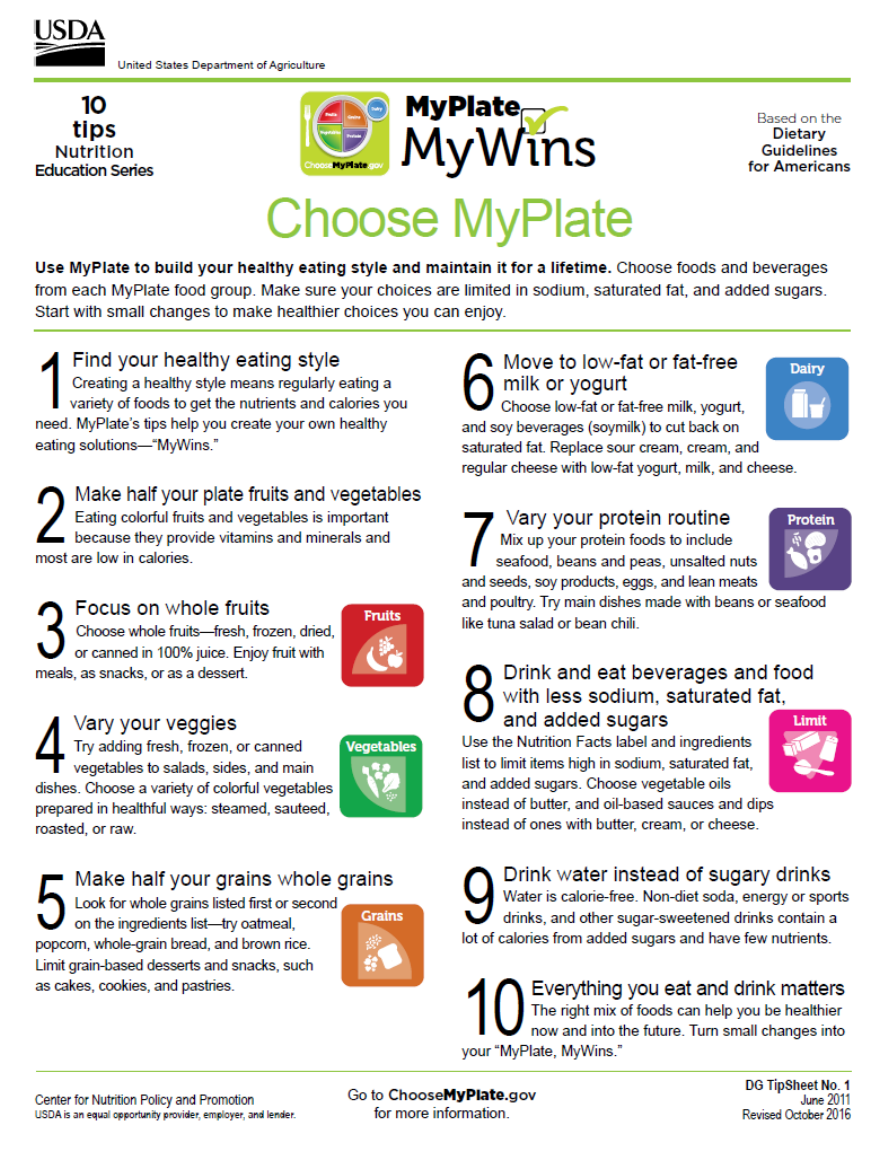
Safe and Effective use of Medications/Food-Drug Interactions;
Nutrition
28
Tobacco Cessation
37
Social Services Department and Community Resources
38
Pocket Inserts:
Health care Associated Infection (HAI) Prevention Program
Hospitalist Program Brochure
Manage Your Health Care with MyChart
Pain Management
Patient Menu
Patient’s Bill of Rights
Post-Operative Pain Management Brochure
Page 1 of 51
Dear Patient,
If you are planning a need for nursing home stay after
discharge from Alomere Health, this notice informs you
that Medicare requires and other insurances may
require a qualifying hospital stay to be eligible for
Nursing Home coverage.
Utilization Review and Social Services will do their best
to provide you with accurate information on Medicare
guidelines for Nursing Home Placement, but financial
coverage is not guaranteed by Alomere Health.
Questions can be directed to:
• Alomere Health Social Services
320-762-6108.
• Alomere Health Utilization Review
320-762-6155.
• Senior LinkAge Line at 1-800-333-2433.
Thank you for your attention,
Alomere Health Social Services and Utilization Review
Page 2 of 51
Outpatient Observation Services Patient’s Guide
What is Observation?
Observation is an outpatient service used to assess, monitor, test and
treat by hospital staff to determine if you will require acute inpatient
services.
What Does this Mean?
This means you will be placed in a room and be observed by the
nursing staff. Although you are in a room and bed and receiving
services similar to inpatients you are not an inpatient.
Why am I an Outpatient Observation Instead of an Inpatient?
Specific criteria must be met in order to admit a patient to the hospital.
In some cases, it is not immediately clear whether a patient is well
enough to go home or if hospitalization is needed. In these cases, a
physician may order outpatient observation care.
Does Outpatient Observation Require a Doctor’s Order?
Yes. A physician’s order is needed to designate the level of
care/service provided to you.
Are there Differences in the Patient Out-Of-Pocket Expenses for
Outpatient Observation?
Yes. The deductible is higher for outpatient observation. There is a
co-insurance amount and some home medications may not be
covered under these services.
How does this Impact my Medicare Coverage?
Outpatient observation stay is not counted as an acute inpatient stay.
Outpatient observation bed services are billed for under Medicare Part
B. You will be financially responsible for applicable co-insurance,
deductible and any other non-covered services.
Is the Hospital Reimbursed for Outpatient Observation Hours?
Yes. Outpatient observation is one of many packaged services paid
for by Medicare. Other medical insurance may pay using your
outpatient benefits. Hospitals need to accurately capture when
outpatient observation begins and to detail all supplies, services, and
tests to ensure appropriate reimbursement.
Page 3 of 51
Outpatient Observation Services Patient’s Guide ~ continued from previous page
When is Outpatient Observation Appropriate?
▪ If you are stable but require further testing and monitoring to define
diagnosis, treatment plan.
▪ Physician feels you will respond rapidly to treatment.
▪ Outpatient surgery patient who develops a complication and require
monitoring or intervention to determine the need for acute inpatient
services.
What are some Presenting Conditions/Symptoms that may be
considered for Outpatient Observation Services?
▪ Abdominal Pain not Requiring Surgery
▪ Anemia
▪ Atrial Fibrillation
▪ Asthma
▪ Back Pain
▪ Cellulitis
▪ Chest Pain
▪ Complications Post Outpatient Surgery
▪ Dehydration
▪ Headache
▪ Heart Failure
▪ Nausea/Vomiting
▪ Observation for any Condition
▪ Pneumonia
▪ Syncope (Fainting)
▪ Transient Ischemic Attack (Small Stroke)
▪ Urinary Tract Infection
▪ Weakness/Dizziness
What Post-Surgery Complications May Warrant Outpatient
Observation Services?
▪ Persistent nausea/vomiting
▪ Uncontrolled pain
▪ Excessive/uncontrolled bleeding
What does NOT Qualify for Outpatient Observation?
▪ Normal outpatient postoperative recovery time.
▪ Diagnostic testing
▪ Continued stay for convenience of patient/family or doctor.
▪ Patient awaiting placement in a long-term facility.
Outpatient Observation Services Patient’s Guide ~ continued from previous page
Page 4 of 51
If my Condition Worsens or I am not Responding to Treatment can I
be Admitted as an Inpatient?
Yes. An outpatient observation service can be converted to inpatient
service at any time by a physician order as long as they meet medical
necessity.
The content in this brochure was adapted by Stratis Health, the Medicare Quality Improvement Organization (QIO) for Minnesota, from information created by Flagler
Hospital and the FMQAI (Florida QIO). March 2008

Page 5 of 51
Patient Rights
It is important that you and your family are aware of your rights.
As a patient of Alomere Health, you have:
•
The right to participate in the development and implementation of your care
plan.
•
The right to have a representative (as allowed under state law) with the right to
make informed decisions regarding your care.
•
The right to be informed of your health status, be involved in care planning and
treatment, and be able to request or refuse treatment. This right must not be
construed as a mechanism to demand the provision of treatment or services
deemed medically unnecessary or inappropriate.
•
The right to formulate advance directives, with confidence that those who
provide care at Alomere Health will comply with these directives.
•
The right to have a family member or representative of your choice, and your
own physician, notified promptly of your admission to the hospital.
•
The right to personal privacy.
•
The right to receive care in a safe setting.
•
The right to be free from all forms of abuse or harassment.
•
The right to confidentiality of your clinical records.
•
The right to access information contained in your clinical records within a
reasonable time frame. The hospital must not frustrate the legitimate efforts of
individuals to gain access to their own medical records and must actively seek
to meet these requests as quickly as its record keeping system permits.
•
The right to be free from restraints of any form that are not medically necessary
or used as a means of coercion, discipline, convenience, or retaliation by staff.
•
The right to be fully informed of, free to consent to, or refuse to participate in
any unusual, experimental or research project without compromising your
access to services.
•
The right to know the professional status of any person providing care or
services.
•
The right to know the reasons for any proposed change in the professional staff
responsible for your care.
•
The right to know the reasons for your transfer either within or outside Alomere
Health.
Page 6 of 51
Patient Rights - Continued from previous page
•
The right to know the relationship(s) of Alomere Health to other persons
or organizations participating in the provision of your care.
•
The right to access the cost, itemized when possible, of services rendered
within a reasonable period of time.
•
The right to be informed of the source of Alomere Health’s reimbursement for
your services, and of any limitations, which may be placed upon your care.
•
The right to have pain treated as effectively as possible.
•
The right to be informed of your visitation rights, including any clinical
restriction
or limitation on such rights (or support person, where appropriate).
•
The right to be informed of the right, subject to your consent, to receive the
visitors whom you designate, including, but not limited to: a spouse, a domestic
partner (including a same sex domestic partner), another family member, or a
friend. This also includes the right to withdraw or deny such consent at any
time (or support person, where appropriate).
•
The right to no restriction, limitation or otherwise denial of visitation
privileges on the basis of race, color, or national origin.
•
The right to assurance that all visitors enjoy full and equal visitation privileges
consistent with patient preferences.
•
The right to provide your family with the right of informed consent for donation
of organs and tissues.
Patient Responsibilities
Just as you have rights as a patient, you also have responsibilities. At Alomere
Health, we believe that you and your health care providers are partners, working
together to reach a common goal – your health, wellness and recovery. Your
responsibilities to us are to:
•
Provide up-to-date, accurate information about your health to members of
your health care team.
•
Ask questions and be sure you understand your treatment plan and medical
condition.
•
Follow the treatment recommended by your physician(s) and other health care
providers.
•
Be considerate of other patients’ rights and privacy.
•
Meet financial obligations to the hospital.
• Observe the ban of tobacco use on the property.

Page 7 of 51
Smoke Free Campus
Notice to Our Patients and Visitors:
Alomere Health is a 100% smoke-free and tobacco-free campus, including all
grounds and facilities. Patients are not allowed to go outside for any reason,
including smoking, even if it is off hospital property. To leave the hospital to smoke, a
patient will need to be discharged. If a patient leaves the hospital before discharge to
smoke, they will be automatically “Discharged Against Medical Advise”. If this
happens, the patient’s insurance may not pay for any of the hospital care.
But We Care About YOU, as a smoker:
The hospital has tobacco and nicotine alternatives to smoking available for you. If
you will be admitted to the hospital, the best thing for you to do is to stop smoking. If
you cannot stop smoking, talk to your provider ahead of time to plan your care and
the use of the alternative for you.
Frequently Asked Questions
Q. Why are we a 100% smoke-free and tobacco-free facility?
A. Smoking and second-hand smoke is widely recognized as the single most
important cause of preventable human disease, including lung cancer, heart
disease and emphysema. Alomere Health and its clinics promote a healthy
environment for all patients, visitors, employees, students and medical trainees.
Q. To whom does this policy apply?
A. The smoke-free and tobacco-free policy applies to ALL employees, patients,
visitors, vendors, students, medical residents and faculty on all property and
grounds owned, leased or operated by Alomere Health.
Q. Where can I smoke?
A. Use of any tobacco product is prohibited on all surrounding Alomere Health
grounds, including all facilities owned, leased or operated by the Alomere Health.
This is a zero-tolerance policy that does not allow smoking or tobacco use on our
property.
Q. I just had a procedure, and I want to leave to have a cigarette. What do I
do?
A. We want to ensure that you have been informed of our smoke-free policy. We
want to work with you to make you comfortable during your stay by providing
information about smoking alternatives. If you leave to smoke, you will be
discharged.
Page 8 of 51
Q. Are electronic cigarettes (e-cigarettes) permitted?
A. The use of e-cigarettes is prohibited. The FDA does not consider e-cigarettes to
be a safe nicotine replacement product or smoking cessation strategy.
Q. As a patient, where can I get help to quit smoking?
A. To help reduce immediate cravings and urges, nicotine replacement products
such as lozenges, gum and patches can be prescribed by your doctor.
There are a variety of resources in the state for smoking cessation, including:
Medications.
Talk to your physician about the following products, which may require a
prescription or need to be purchased by patient:
Bupropion (Zyban)
Nicotine Patch
Nicotine Gum
Nicotine Spray
Nicotine Inhaler
Varenicline (Chantix)
Nicotine Lozenge
Q. What should I do if I observe someone smoking?
A. Contact the Visitor Information Desk in the main lobby and inform them, or tell
security personnel if they are available. The individual(s) who are smoking will
be politely informed of the policy.
Q. Are other health care facilities smoke-free?
A. Smoking and second-hand smoke is widely recognized as the single most
important cause of preventable human disease, including lung cancer, heart
disease and emphysema. The decision to prohibit smoking is an issue that all
U.S. hospitals are facing and are increasingly choosing as a healthy option for
their patients, visitors and employees.
Tobacco Quit Line Available at 1-800-QUIT-NOW (784-8669), seven days a
week, 7:00 am-11:00 pm

Page 9 of 51
Privacy Practices
The Federal Health Information Portability and Accountability
Act (HIPAA) and Minnesota Law require that we protect your
Health Information.
The nursing staff wants you to be aware of the new
regulations that affect how we use and disclose your health
information. Please review the following guidelines on how
we may share this information.
● Phone calls will be transferred to the patient/family if
appropriate. They may share the information they
choose.
● If a caller or visitor asks for the patient by name, we
may disclose minimal information about your
hospitalization.
● The nursing staff will make a reasonable effort to
protect your health information. There may be special
circumstances when a caller/visitor needs to obtain
information from the nursing staff. We then will request
two contact names to release minimal information.
Thank you for your cooperation and understanding.
Alomere Health Nursing Staff.

Page 10 of 51
Contacting Your Family Physician
You have the right to ask us to contact your family physician of
this hospital visit. This does not mean your family physician
will automatically assume care for you while hospitalized.
Please notify your nurse if you would like us to inform your
family physician of this hospital visit.

Page 11 of 51
The Grievance Process at
Alomere Health
A patient grievance is a formal, written or verbal grievance or complaint
that is filed by a patient when a patient issue cannot be resolved
promptly by staff.
To file a patient grievance at Alomere Health, you may either utilize the
hospital’s process or contact the State Agency directly.
The grievance process at Alomere Health may be implemented several
ways. You may notify your nurse, the charge nurse on your unit, or the
Nursing Supervisor. The Nursing Supervisor can be reached by dialing
“0” to the switchboard operator and asking them to page the Nursing
Supervisor so you can speak with the Nursing Supervisor directly.
The State Agency you may contact includes any one of the following:
Minnesota Board of Medical Practice
2829 University Ave. SE, Suite 500
Minneapolis MN 55414-3246
(612) 617-2130
(800) 657-3709
Office of Health Facility Complaints
85 E Seventh Place
PO Box 64970
St. Paul MN 55164-0970
(651) 201-4200
(800) 369-7994
Office of Ombudsman for Older Minnesotans
PO Box 64971
St. Paul MN 55164-0971
(651) 431-2555
(800) 657-3591
Page 12 of 51
Help Protect People who are Frail or Vulnerable
Take Action – Call and Report - 1-844-880-1574
Vulnerable Adults Need Your Help
You notice that your elderly friend Gladys no longer has money for personal
things. Her daughter has taken control of her checkbook and Gladys does not
know what happens to her Social Security check.
You come to visit your dad, and you notice there is not any food in the house, he
is unkempt, and you are worried that he is not taking his medications.
What should you do?
You need to report these types of cases so that these vulnerable adults can get the
protection and safety they need.
Vulnerable adults have an impaired ability to provide for their own needs and protect
themselves from harm. The law can protect and assist them.
Many vulnerable adults are reluctant to report, and when asked about it directly they
may even deny that harm occurred. That is why it is so important for family members,
friends, physicians, social workers and others to be aware of abuse, neglect and
exploitation and report if you suspect something is going on.
If you are a mandated reporter under the law, you MUST report suspected
harm.
Who is at risk?
People who depend on others for care or assistance in daily living have a higher risk
of being harmed. Some people have a higher risk of harm by simply being elderly,
frail or disabled.
Harm can occur anywhere by any one.
Abuse, neglect and exploitation can occur anywhere, from a person’s own home to a
nursing home, from an assisted living facility to an adult day program.
Abusers include spouses, children, staff, as well as “self.” Vulnerable adults may no
longer be able to care for themselves, and so are in danger of “self-neglect.” By
calling the Common Entry Point, you can help the vulnerable person get much
needed assistance.
For more information about the law, reporting maltreatment of a vulnerable
adult, or Adult Protection Services, please call your local county social
services agency or the Minnesota Department of Human Services Adult
Services Unit, 651-431-2547 or 651-431-2609.
Call to report abuse, neglect or exploitation of a vulnerable person
If there is immediate danger to the vulnerable adult, call 911 immediately. If you
suspect abuse, neglect or financial exploitation, you should call your county’s
designated “Common Entry Point.” The Common Entry Point receives all reports of
known or suspected maltreatment and works with appropriate authorities.
The phone line is available 24 hours a day/7 days a week, so reports can be taken
immediately.
Page 13 of 51
Help Protect People who are Frail or Vulnerable ~ continued from previous page
Minnesota Common Entry Point:
1-844-880-1574
Other important numbers to know:
Immediate or serious danger, call 911.
The State Office of Ombudsman for Long Term Care 651-431-2555 or
toll free at 800-657-3591.
Elder Care Rights Alliance 952-854-7304.
Senior LinkAge Line™ 1-800-333-2433.
What are the warning signs of abuse?
The person may say that she is being harmed or he is afraid of someone.
Bruises and skin tears.
Black eyes.
Broken bones.
Burns or cuts.
Internal injuries.
Infections
Changes in mental functioning or behavior (such as increased agitation,
combativeness, depression or confusion)
Injuries that are unexplained or are not consistent with the explanation given.
What are the warning signs of neglect?
Dehydration, weight loss & malnutrition.
Pressure sores, poor hygiene.
Depression, confusion or other changes in mental functioning.
Absence of needed medical equipment or prostheses.
Repeated falls.
Incontinence, isolation.
What are the warning signs of financial exploitation?
The person may say something like, “I don’t know anything about it, my
son/daughter/friend handles all my business.”
Bills go unpaid.
The person does not have access to their own money.
The person is asked to sign documents but does not know what they are.
Changes are made in the will.
Assets are transferred or sold.
The person is taken to the bank to make account withdrawals.
Personal property, like cash, checks, credit cards, jewelry, furniture, etc., is
missing.
This information is available in other forms to people with disabilities by
contacting us at 651-431-2500 (voice) or toll free at 800-882-6262. TTY/TDD
users can call the Minnesota Relay Service at 711 or 800-627-3529. For the
Speech-to-Speech Relay, call 877-627-3848.
For serious or immediate danger,
call 911.

Page 14 of 51
Minnesota Department of Health
Questions and Answers About Health Care Directives
Return to Information Bulletin 98-4
Minnesota Law
Minnesota law allows you to inform others of your health care wishes. You have
the right to state your wishes or appoint an agent in writing so that others will know
what you want if you can't tell them because of illness or injury. The information
that follows tells about health care directives and how to prepare them. It does not
give every detail of the law.
What is a Health Care Directive?
A health care directive is a written document that informs other of your wishes
about your health care. It allows you to name a person ("agent") to decide for you
if you are unable to decide. It also allows you to name an agent if you want
someone else to decide for you. You must be at least 18 years old to make a
health care directive.
Why Have a Health Care Directive?
A health care directive is important if your attending physician determines you
can't communicate your health care choices (because of physical or mental
incapacity). It is also important if you wish to have someone else make your health
care decisions. In some circumstances, your directive may state that you want
someone other than an attending physician to decide when you cannot make your
own decisions.
Must I Have a Health Care Directive? What Happens if I Don't
Have One?
You don't have to have a health care directive. But, writing one helps to make sure
your wishes are followed.
You will still receive medical treatment if you don't have a written directive. Health
care providers will listen to what people close to you say about your treatment
preferences, but the best way to be sure your wishes are followed is to have a
health care directive.
How Do I Make a Health Care Directive?
There are forms for health care directives. You don't have to use a form, but your
health care directive must meet the following requirements to be legal:
• Be in writing and dated.
• State your name.
Page 15 of 51
Questions and Answers about Health Care Directives – continued from previous page
• Be signed by you or someone you authorize to sign for you, when you can
understand and communicate your health care wishes.
• Have your signature verified by a notary public or two witnesses.
• Include the appointment of an agent to make health care decisions for you
and/or instructions about the health care choices you wish to make.
Before you prepare or revise your directive, you should discuss your health care
wishes with your doctor or other health care provider.
Information about how to obtain forms for preparation of your health care directive
can be found in the Resource Section of this document.
I Prepared My Directive in Another State. Is It Still Good?
Health care directives prepared in other states are legal if they meet the
requirements of the other state's laws or the Minnesota requirements. But requests
for assisted suicide will not be followed.
What Can I Put in a Health Care Directive?
You have many choices of what to put in your health care directive. For example,
you may include:
• The person you trust as your agent to make health care decisions for you.
You can name alternative agents in case the first agent is unavailable, or
joint agents.
• Your goals, values and preferences about health care.
• The types of medical treatment you would want (or not want).
• How you want your agent or agents to decide.
• Where you want to receive care.
• Instructions about artificial nutrition and hydration.
• Mental health treatments that use electroshock therapy or neuroleptic
medications.
• Instructions if you are pregnant.
• Donation of organs, tissues and eyes.
• Funeral arrangements.
• Who you would like as your guardian or conservator if there is a court
action.
You may be as specific or as general as you wish. You can choose which issues
or treatments to deal with in your health care directive.
Are There Any Limits to What I Can Put in My Health Care
Directive?
There are some limits about what you can put in your health care directive. For
instance:
• Your agent must be at least 18 years of age.
• Your agent cannot be your health care provider, unless the health care
provider is a family member or you give reasons for the naming of the agent
in your directive.
Page 16 of 51
Questions and Answers about Health Care Directives – continued from previous page
• You cannot request health care treatment that is outside of reasonable
medical practice.
• You cannot request assisted suicide.
How Long Does a Health Care Directive Last? Can I Change It?
Your health care directive lasts until you change or cancel it. As long as the
changes meet the health care directive requirements listed above, you may cancel
your directive by any of the following:
• A written statement saying you want to cancel it.
• Destroying it.
• Telling at least two other people you want to cancel it.
• Writing a new health care directive.
What If My Health Care Provider Refuses to Follow My Health
Care Directive?
Your health care provider generally will follow your health care directive, or any
instructions from your agent, as long as the health care follows reasonable
medical practice. But, you or your agent cannot request treatment that will not help
you or which the provider cannot provide. If the provider cannot follow your agent's
directions about life-sustaining treatment, the provider must inform the agent. The
provider must also document the notice in your medical record. The provider must
allow the agency to arrange to transfer you to another provider who will follow the
agent's directions.
What If I've Already Prepared a Health Care Document? Is It Still
Good?
Before August 1, 1998, Minnesota law provided for several other types of
directives, including living wills, durable health care powers of attorney and mental
health declarations.
The law changed so people can use one form for all their health care instructions.
Forms created before August 1, 1998, are still legal if they followed the law in
effect when written. They are also legal if they meet the requirements of the new
law (described above). You may want to review any existing documents to make
sure they say what you want and meet all requirements.

Page 17 of 51
Questions and Answers about Health Care Directives – continued from previous page
What Should I Do with My Health Care Directive After I Have
Signed It?
You should inform others of your health care directive and give people copies of it.
You may wish to inform family members, your health care agent or agents, and
your health care providers that you have a health care directive. You should give
them a copy. It's a good idea to review and update your directive as your needs
change. Keep it in a safe place where it is easily found.
What if I believe a Health Care Provider Has Not Followed Health
Care Directive Requirements?
Complaints of this type can be filed with the Office of Health Facility Complaints at
651-201-4200 (Metro Area) or Toll-free at 1-800-369-7994.
What if I Believe a Health Plan Has Not Followed Health Care
Directive Requirements?
Complaints of this type can be filed with the Minnesota Health Information
Clearinghouse at 651-201-5178 or Toll-free at 1-800-657-3793.
How to Obtain Additional Information
If you want more information about health care directives, please contact your
health care provider, your attorney, or:
Minnesota Board on Aging's Senior LinkAge Line®
1-800-333-2433.
A suggested health care directive form is available on the internet at:
http://www.mnaging.org/.

Page 18 of 51
Patient Information
Safe Patient Handling
Alomere Health uses special lifting equipment and/or moving
aides to safely transfer patients with limited mobility. The use
of safe patient moving equipment helps better protect patients
from skin injuries, falls and provides comfort when patients
are being moved. This equipment also reduces injuries to
hospital caregivers.
Our staff will show you how the equipment works. Please
share any question or concerns you may have with your care
team.
Your safety is very important to us. We hope to make you as
comfortable as possible during your hospital stay.
Page 19 of 51
Venous Thrombosis Embolism (VTE)
Information and Discharge Education
Vein Thrombosis Embolism (VTE) is a blood clot which forms in a deep vein, which is
commonly located in a leg. The danger of VTE is that it can shut off blood flow to that
area or the clot can break apart and travel to other organs. A clot which reaches the lungs
is called a pulmonary embolism; this can be a life-threatening event.
Conditions which can increase risk to develop a VTE are:
• Age > 40 years
• Cancer
• Clotting disorder
• Estrogen or oral contraceptive use
• Immobility
• Inflammatory diseases
• Obesity
• Pregnancy
• Previous VTE
• Surgery
VTE may occur without symptoms or may produce severe pain, fever, malaise and
swelling of affected arm or leg. The number one symptom is edema of affected limb in
which the onset is sudden.
Symptoms of Pulmonary Embolism include:
• Chest Pain
• Cough
• Fever
• Rapid Heartbeat
• Shortness of Breath
VTE Prevention Measures:
• Range of motion leg exercises every hour while in bed.
• Avoid long periods of sitting or standing.
• Short periods of walking every 2 hours.
Treatment:
If you are diagnosed with VTE, medications such as Coumadin (Warfarin) can be
prescribed to prevent clot formation. These medications do not dissolve clots, but rather
prevent future clots from forming. All of these medications may cause bleeding and can
only be taken when prescribed by your physician.
If discharge medications include blood thinners such as Coumadin (Warfarin), consider
the following:
• There are many medicines you should avoid while using blood thinners. These
include many herbs, supplements, and over-the-counter medicines. Ask your doctor
before using other medicines, especially products that contain nonsteroidal anti-
inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, naproxen, Advil®, Aleve®, or
Motrin®. Carefully check the labels of all other medicines to be sure they do not
contain NSAIDs.

Page 20 of 51
Venous Thrombosis Embolism (VTE) ~ continued from previous page
• Carefully follow your doctor’s instructions about any special diet. This medicine works
best when you eat the same amount of vitamin K in your food every day. Avoid big
changes in how much vitamin K you eat. Some foods that have a high amount of
vitamin K are asparagus, broccoli, Brussel sprouts, cabbage, green leafy vegetables
(such as collards, turnip greens, mustard greens, spinach, and salad greens), plums
and certain vegetable oils (such as soybean oil and canola oil).
• Avoid drinking cranberry juice or any other cranberry products.
• Do not drink alcohol while you are using this medicine.
• It is very important to have regular doctor visits post-hospital discharge. Blood tests,
such as INR, are needed to check for proper dosage and unwanted side effects.
Page 21 of 51
Preventing Skin Breakdown
What is a pressure ulcer?
A pressure ulcer or bedsore is an injury to the skin and the tissue beneath it. It
is caused by pressure on the skin. Pressure ulcers can slow your recovery,
causing pain, infections and other problems. Pressure ulcers tend to occur
over bony body parts (elbow, heel, hip, etc.) that you sit or lie on for long
periods of time. The pressure squeezes tiny blood vessels that supply the skin
with nutrients and oxygen. When skin goes without nutrients and oxygen for
too long, a pressure ulcer forms.
Pressure ulcers are more likely to develop or worsen in the following situations:
• Sliding down in a bed or chair.
• Rubbing or creating friction on the skin.
• Inability to change positions.
• Loss of bowel or bladder control.
• Inadequate nutrient or fluid intake.
• Poor circulation or fragile skin.
• Inability to think clearly.
• Inability to feel pain or pressure.
Preventing pressure ulcers
• Limit pressure.
o If you are in bed, change your position at least every one to two
hours.
o If you are in a chair and can shift your own weight, do so every 15
minutes. If you cannot shift your own weight, your caregiver should
change your position at least every hour.
• Reduce friction.
o When moving in bed, do not pull or drag yourself across the sheets
and do not push or pull with your heels.
o Avoid repetitive movements. For example, don’t scratch your foot by
rubbing it on the sheets.
• Use padding carefully.
o Avoid doughnut-shaped cushions. These can hurt the tissues under
your skin.
o Avoid using several layers (such as underpads, diapers and sheets)
between you and your chair or bed.
• Protect your skin.
o Have someone check your skin often. Tell your care provider if
anything looks unusual.
o Clean your skin well after using a bedpan or soiling a diaper or pad.
o Use moisturizer to prevent dry skin. Bathe every other day.
o Do not rub or massage the skin over the bony parts of your body.
Hydration
Dehydration can increase your risk of skin breakdown. To avoid dehydration,
drink small sips throughout the day and keep a water bottle nearby at all times.
Page 22 of 51
Preventing Skin Breakdown ~ continued from previous page
If you must stay in bed for long periods of time:
• Keep the head of your bed as low as you can. If you need to raise it, raise it
to the lowest point possible for as short a time as possible.
• Use pillows to keep your knees and ankles from touching each other.
• Avoid lying directly on your hipbone when on your side.
• Keep your heels off the bed, place pillows under your legs from mid-calf to
ankle. Never place pillows under the knee.
If you have problems with bladder or bowel control:
• Only use pads made for incontinence (these pull moisture away from your
skin).
• Clean the skin gently with a pH-balanced soap or cleansing product.
If you are often in a chair or wheelchair:
• Remember that comfort and good posture are important.
• Change your position often. Spend time out of the chair several times a
day.
Devices and Pressure Ulcers
Devices such as anti-embolism stockings, cervical collars, back braces, splints,
oxygen tubing and oxygen masks can cause pressure and skin breakdown. To
avoid device related pressure ulcers:
• Inspect areas of skin where devices are applied.
• Inspect between skin folds.
• Observe tension of straps and tubings and make adjustments.
• Inspect skin daily.
• Contact your physician for non-healing areas or unusual drainage from
wound.
• Inform staff if you experience pain or discomfort beneath or around the
device.
Skin Health and Diet ~ Healing Snacks
Foods that have high amounts of protein and certain vitamins and minerals
may help improve healing.
Protein:
Meat, beans, cheese, peanut butter, eggs, milk, cottage cheese, and
yogurt.
Vitamin A:
Liver, egg yolks, deep green, yellow and orange fruits and vegetables.
Zinc:
Shellfish, oatmeal, spinach, nuts, and meats.
Iron:
Liver, sardines, tuna, raisins, dried prunes, dried peaches, and dried
beans.
Vitamin E:
Meat, whole grains, green leafy vegetables, and egg yolks.
Vitamin C:
Citrus fruits, orange juice, tropical fruit such as papaya, mango or guava,
red or green peppers, dark green leafy vegetables, potatoes, cabbage,
cantaloupe and strawberries.

Page 23 of 51
Call Before You Fall
A Guide to Fall Prevention
Fall Prevention Information
Alomere Health is committed to patient safety which includes fall prevention.
During your stay at Alomere Health, the staff will be continually assessing your
risk for falls based on your medical condition and risk factors.
Falls can occur frequently and are a major cause of disability and death in the
elderly. Thirty percent of individuals over 65 years of age fall annually.
Injuries from falls can range from minor bruising to life threatening trauma.
Head injuries and fractures of the long bones are often the most life
threatening.
Where Do Falls Occur?
60% occur at home
30% occur in community
10% occur in institutions
Risk Factors for Falls:
Greater than 65 years of age and ages 1-4 years
History of past falls
Blood thinner medications
Taking multiple medications for various medical conditions
Acute illness or surgery
Poor hearing and vision
Use of aids such as canes, walkers, etc.
To Prevent Falls During Your Hospitalization:
Wear shoes or non-skid slippers every time you get out of bed.
Call your nurse if you feel dizzy, weak, lightheaded or if you have fallen. Do
not get up by yourself.
Ask for help to go to the bathroom. Make sure the path to the bathroom is
clear.
Use only unmoving objects to help steady yourself. Do not use your IV
pole, tray table, wheelchair or other objects that can move.
Use the handrails in the bathroom and hallway.
If you wear glasses or hearing aids, use them.
Keep important items within reach. This includes your call button.
To Prevent Falls at Home:
Lighting:
Make sure that you have good, bright lighting in your home. Use night-
lights in your bedroom, hall and bathroom.
Keep flashlight available.
Page 24 of 51
Call Before You Fall ~ continued from previous page
Rugs:
Make sure rugs are firmly fastened to the floor or use nonskid backing.
Remove scatter rugs.
Electrical Cords:
Move electrical cords so they are not lying on the floor in walking areas.
Bathroom:
Put handrails in your bathroom for bath, shower, and toilet use.
Use a raised toilet seat.
Place nonskid strips in tub.
Stairs/Stairwells:
Always use handrails for support. Be sure the stairs are well lit.
Remove clutter from stairs.
Kitchen:
Store items within easy reach. Avoid using stepstools or stepladders.
Wipe spills immediately.
Footwear:
Wear shoes with firm non-skid, non-friction soles.
Avoid wearing loose-fitting slippers.
Phone:
Keep phone within easy reach.
What Else Can I Do?
See your eye doctor once a year.
Take good care of your feet and have them examined if you have pain or
difficulty walking.
Talk to your doctor about any side affects you may have with your
medicines. Some side effects may contribute to falls.
See your doctor if you have dizzy spells.
A cane or walker will provide extra stability when walking and may help to
avoid a fall.
When getting out of bed, sit on the side of the bed for a few minutes before
standing up. Your blood pressure takes some time to adjust when you sit
or stand up. If you move too quickly, you can become dizzy and this
increases your chances of falling.
Tell your doctor if you fall—medical evaluation can help!
If you do Fall:
Notify your healthcare provider or call 911 if you have been injured. Be
sure to report use of blood thinning medication.
Report symptoms of headache, dizziness, nausea, weakness, confusion or
significant bleeding.
Page 25 of 51
What You Can Do to Stay Safe
20 Tips to Help Prevent Medical Errors
The best way you can help to prevent errors is to be an active member of your health care
team. That means taking part in every decision about your health care. Research shows
that patients who are more involved with their care tend to get better results.
Medicines
1. Make sure that all of your doctors know about every medicine you are taking.
This includes prescription and over-the-counter medicines and dietary supplements,
such as vitamins and herbs.
2. Bring all of your medicines and supplements to your doctor visits. This
includes medications given as intravenous infusions. Please let your doctor
know if you have had any immunizations in the last 30 days.
"Brown bagging" your medicines can help you and your doctor talk about them and
find out if there are any problems. It can also help your doctor keep your records up
to date and help you get better quality care.
3. Make sure your doctor knows about any allergies and adverse reactions you
have had to medicines.
This can help you to avoid getting a medicine that could harm you.
4. When your doctor writes a prescription for you, make sure you can read it.
If you cannot read your doctor's handwriting, your pharmacist might not be able to
either.
5. Ask for information about your medicines in terms you can understand—both
when your medicines are prescribed and when you get them:
What is the medicine for?
How am I supposed to take it and for how long?
What side effects are likely? What do I do if they occur?
Is this medicine safe to take with other medicines or dietary supplements I
am taking?
What food, drink, or activities should I avoid while taking this medicine?
6. When you pick up your medicine from the pharmacy, ask: Is this the medicine
that my doctor prescribed?
7. If you have any questions about the directions on your medicine labels, ask.
Medicine labels can be hard to understand. For example, ask if "four times daily"
means taking a dose every 6 hours around the clock or just during regular waking
hours.
Page 26 of 51
What You Can Do to Stay Safe ~ continued from previous page
8. Ask your pharmacist for the best device to measure your liquid medicine.
For example, many people use household teaspoons, which often do not hold a true
teaspoon of liquid. Special devices, like marked syringes, help people measure the
right dose.
9. Ask for written information about the side effects your medicine could cause.
If you know what might happen, you will be better prepared if it does or if something
unexpected happens.
Hospital Stays
10. If you are in a hospital, consider asking all health care workers who will touch
you whether they have washed their hands.
Handwashing can prevent the spread of infections in hospitals.
11. When you are being discharged from the hospital, ask your doctor to explain
the treatment plan you will follow at home.
This includes learning about your new medicines, making sure you know when to
schedule follow-up appointments, and finding out when you can get back to your
regular activities.
It is important to know whether or not you should keep taking the medicines you were
taking before your hospital stay. Getting clear instructions may help prevent an
unexpected return trip to the hospital.
Surgery
12. If you are having surgery, make sure that you, your doctor, and your surgeon
all agree on exactly what will be done.
Having surgery at the wrong site (for example, operating on the left knee instead of
the right) is rare. But even once is too often. The good news is that wrong-site
surgery is 100 percent preventable. Surgeons are expected to sign their initials
directly on the site to be operated on before the surgery.
13. If you have a choice, choose a hospital where many patients have had the
procedure or surgery you need.
Research shows that patients tend to have better results when they are treated in
hospitals that have a great deal of experience with their condition.
Other Steps
14. Speak up if you have questions or concerns.
You have a right to question anyone who is involved with your care.
Page 27 of 51
What You Can Do to Stay Safe ~ continued from previous page
15. Make sure that someone, such as your primary care doctor, coordinates your
care.
This is especially important if you have many health problems or are in the hospital.
16. Make sure that all your doctors have your important health information.
Do not assume that everyone has all the information they need.
17. Ask a family member or friend to go to appointments with you.
Even if you do not need help now, you might need it later.
18. Know that "more" is not always better.
It is a good idea to find out why a test or treatment is needed and how it can help you.
You could be better off without it.
19. If you have a test, do not assume that no news is good news.
Ask how and when you will get the results.
20. Learn about your condition and treatments by asking your doctor and nurse
and by using other reliable sources.
For example, treatment options based on the latest scientific evidence are available
from the Effective Health Care Web site
(
http://www.effectivehealthcare.ahrq.gov/options). Ask your doctor if your treatment is
based on the latest evidence.
*The term "doctor" is used in this flier to refer to the person who helps you manage your health
care.
AHRQ Publication No. 11-0089
Replaces AHRQ Publication No. 00-P038
Current as of September 2011
Internet Citation:
20 Tips to Help Prevent Medical Errors. Patient Fact Sheet. AHRQ Publication No. 11-0089,
September 2011. Agency for Healthcare Research and Quality, Rockville, MD.
http://www.ahrq.gov/consumer/20tips.htm
Page 28 of 51
Safe and Effective Use of Medications
What are Medications?
Medications are used to prevent and treat diseases and disorders and to relieve
pain and discomfort. For your own safety, health, and well-being, it is important that
you learn about the safe and effective use of your specific medication.
What Should You Know About Your Medication?
1. Know why you take your medication - some medicines have many uses -
know what you take it for.
2. Know how to take your medication - how much, at what specific times of
day, with or without food.
3. Know for how long to take your medication. Some medications should be
taken for a specific amount of time, others for a lifetime.
4. Take medications as prescribed by your physician.
5. Get your prescription refilled before your supply is gone.
6. Check with your physician or pharmacist before taking non-prescription
drugs. These are medications and should not be taken carelessly.
7. Report promptly any side effects, or unusual reactions to the medication, to
your physician.
8. Use aids to remember your times - a written schedule, a calendar, an alarm
clock or watch.
9. Understand what the directions on your medication mean.
10. Keep all medications out of reach of children.
11. Remember to obtain enough medication to last for trips and vacations.
12. Don't take anyone else's medication or allow anyone else to take your
medication.
13. Follow all printed instructions given to you for specific medications
concerning proper storage, expiration, and disposal of expired or unused
medications.

Page 29 of 51
Safe and Effective Use of Medications ~ continued from previous page
Why is it Important to Take Your Medication?
Not taking your medication when your doctor thinks you are, may lead to he/she
prescribing more medications because the desired effect of the medication has not
occurred. This extra prescribing will amount to extra cost to you and a risk of side
effects from another medication. Deciding to suddenly stop taking medication that
you have been taking, can lead to ill effects - for example, a person with coronary
artery disease who has been taking propranolol and suddenly stops the drug could
experience an episode of angina or even a heart attack.
Filling Your Prescription:
Choosing a Pharmacy:
Consider not only price and convenience (close to home or delivery service), but
also how well the pharmacist answers your questions. Many pharmacies will keep
a list of all your medicines to be sure you aren't taking medicines that shouldn't be
taken together. You should expect to receive written medication instructions from
your pharmacist. If you don't receive written instructions, contact your pharmacist
or Alomere Health Pharmacy at 762-6029.
Cost of Your Medicine:
First of all, consider if you can afford not to take it. Is it less expensive to take $20
of medicine a month or to miss a month of work because you are sick and pay for
a doctor's visit also?
There are several ways you may be able to reduce the cost of your prescription:
1. If your doctor agrees to it, a generic drug may be available and may cost
less. However, you should usually continue with the same generic
product once you start taking it.
2. Medications are often eligible for insurance coverage after a deductible is
met. Check with your insurance.
3. Check with your pharmacy - they may offer senior citizen or other
discounts.
4. Check with your doctor - a lower cost drug might be available that would
treat your disorder.
5. Many drug companies and foundations may offer copay assistance
programs. Please check with your doctor, pharmacist or social worker to
see if you may be eligible for any of these programs.
Child resistant containers are required by law for most medicines and should be
used if there are small children in your household. However, if you have trouble
opening your medicine, you may request a regular cap on your medicine from your
pharmacist.
Page 30 of 51
Most Frequent and Potential Food
and Drug Interactions
Abbreviated Guide to Food and Drug Interactions
Anticonvulsants (Tegretol) and Generic - Carbamazepine
Possible dietary side effects: Nausea, vomiting, diarrhea, constipation, altered taste,
loss of appetite, inflammation of the mouth (including lips, tongue and mucous
membranes).
Recommendations: Take with food
Anticoagulants (Warfarin) - Brands Coumadin or Jantoven.
Possible dietary side effects: Increased absorption with food except Vitamin K.
Too much alcohol or grapefruit products can increase Warfarin’s effect.
High protein low carbohydrate diets to lose weight can cause a decrease in
Warfarin available so the Warfarin dose may need to be adjusted.
Recommendations: Keep Vitamin K food intake constant. High Vitamin K foods
include: Broccoli, spinach, cabbage, Brussel sprouts, collard greens, cauliflower, liver,
endive, kale, Swiss chard, soybeans, sauerkraut, lettuce, lentils, mustard greens,
turnip greens, garbanzo beans, hummus, canola oil, soybean oil and mayonnaise,
asparagus, avocado, coleslaw.
Anticonvulsant (Dilantin) - Generic - Phenytoin
Possible dietary side effects: Nausea, vomiting, constipation, altered taste,
decreased bone density, cause megaloblastic anemia, decreased serum folate,
decreased copper.
Recommendations: Take with food. Increase fiber and fluids. No alcohol.
Antiarrhythmic Lanoxin (Digoxin) or Antihyperlipidemic drugs such as:
Atorvastatin (Lipitor)
Colesevelam (Welchol)
Ezetimibe (Zetia)
Ezetimibe/Simvastatin (Vytorin)
Fluvastatin (Lescol)
Gemfibrozil (Lopid)
Lovastatin (Mevacor)
Pravastatin (Pravachol)
Rosuvastatin (Crestor)
Simvastatin (Zocor)
Possible dietary side effects: High fiber diets may cause drugs to bind to fiber.
Recommendations: Separate fiber from drug by several hours.
Page 31 of 51
Most Frequent and Potential Food and Drug Interactions ~ continued from previous page
Blood Pressure Drugs
Possible dietary side effects - Avoid natural licorice. It contains glycyrrhiza, which,
when eaten in large amounts, may lead to water retention and drive up blood
pressure.
Benazepril (Lotensin)
Candesartan (Atacand)
Captopril (Capoten)
Chlorothiazide (Diuril)
Enalapril (Vasotec)
Lisinopril (Zestril, Prinivil)
Losartan (Cozaar)
Methyldopa (Aldomet)
Propranolol (Inderal)
Ramipril (Altace)
Valsartan (Diovan)
Recommendations: Artificially flavored licorice is a safer choice.
Gastrointestinal Agents (Mylanta) - Aluminum Hydroxide/Magnesium Hydroxide
Possible dietary side effects: May cause constipation.
Recommendations:
One hour after meals and bedtime.
Follow nursing administration time not to be given at same time
as antibiotics.
MAO Inhibitors not used at Alomere Health very often but significant food drug
interaction.
Selegiline (Eldepryl)
Isocarboxazid (Marplan)
Phenelzine (Nardil)
Tranlcypromine (Parnate)
Possible dietary side effects - Elevated blood pressure, headache, nausea, vomiting,
abnormally rapid heartbeat, loss of appetite, constipation. Increased appetite with
weight gain.
Recommendations – Avoid high tyramine foods: aged cheese, dairy products close
to their expiration date, banana peels, tofu, tap beer, soy sauce, excess caffeine and
alcohol, bean curd, aged protein foods such as sausage/pepperoni/salami/corned
beef, sauerkraut, fava beans, broad green pods, improperly stored pickled herring,
concentrated yeast extracts (Marmite), or any food that has become spoiled or over-
ripened (no over-ripe bananas). Caution with herbal teas as they may contain
tyramine.
Antibiotic (Tetracycline, Ciprofloxacin and Levofloxacin) not used at Alomere Health very
often but significant food drug interaction.
Possible dietary side effects - Nausea, vomiting, loss of appetite, diarrhea,
inflammation of the tongue, (calcium, iron, magnesium, and zinc) inhibit absorption.
Decreased Vitamin K production. Increased need for riboflavin and ascorbic acid.

Page 32 of 51
Most Frequent and Potential Food and Drug Interactions ~ continued from previous page
Recommendations:
Avoid dairy products one hour before or after.
If taking a calcium supplement or multi-vitamin with minerals, take
Tetracycline antibiotic two hours before or six hours after.
Follow the same recommendations for Doxycycline (Vibramycin) and
Demeclocycline (Declomycin) also.
References: Zaneta M. Pronsky, “Food Medications Interactions,” “Pharmacist’s Letter/Prescriber’s Letter,”
“Stay Well” by KRAMES
Academy of Nutrition and Dietetics, Web-based Nutrition Care Manual

Page 33 of 51
Herbal Supplement Interactions
Medical supervision is suggested with herbal supplementation therapy.
Herbal supplements may:
Interact with medications, interfere with prescribed medication actions and
may cause increased side effects.
Affect blood glucose levels.
Lack of regulation of the herbal supplement industry causing variations in
labeled concentrations.
Food-drug interactions with Warfarin medication.
Interfere with anesthesia or heart functioning that increase the risk of
complications during surgery.
Diminish appetite in growing children.
Some herbs are considered unsafe during breast-feeding.
Some may be dangerous alternative remedies.
Herbal therapy is not allowed while you are a patient at Alomere
Health.
Discontinue all herbs two to three weeks before surgery as they may
prolong the effects of anesthesia, increase bleeding and cause
fluctuations in blood pressure.
References:
1. American Society of Anesthesiologists: Herbal Products Warning.
www.asahq.org/patient education/iusidherb.html.
2. Herbal Medicines can interfere with Surgery. Tufts University Newsletter
2001;08-31.
3. Natural Medicines Comprehensive Database at
www.naturaldatabase.com.
4. Academy of Nutrition and Dietetics. Nutrition Care Manual at
https://www.nutritioncaremanual.org.
Page 34 of 51
Potential Grapefruit and Drug Interactions
Many drugs interact with grapefruit juice, grapefruit segments or an extract of
unprocessed grapefruit by increasing blood concentrations of several drugs.
Flavonoids, which are found in grapefruit but not in commercial orange juice,
inhibit the drug metabolizing enzymes. Increased drug levels may cause more
side effects and/or toxicity. Avoid grapefruit and grapefruit juice with the
following drugs:
Anti-Anxiety
Buspirone (BuSpar)
Sertraline (Zoloft)
Clomipramine (Anafranil)
Cardiac Drugs
Carvedilol (Coreg)
Anti-Convulsant
Carbamazepine (Carbatrol,Tegretol)
Claudication Reduction
Cilostazol (Pletal)
Anti-Fungal
Intraconazole (Sporanox)
Cough Suppressants
Dextromethorphan (Benylin, Pertussin,
Robitussin)
Antiarrhythmic
Amiodarone (Cordarone)
Immuno-Suppressants
Cyclosporine (Neoral, Sandimmune)
Tacrolimus (Prograf)
Sirolimus (Rapamune)
Antihistamines
Fexofenadine (Allegra)
Erectile Dysfunction
Sildenafil (Viagra)
Vardemafil (Levitra)
Antiretroviral
Indinavir Sulfate (Crixivan)
Estrogens
Estrogenic Substance (Premarin)
Benzodiazepines
Diazepam (Valium), Midazolam
Triazolam (Halcion), Alprazolam (Xanax)
HMG - CoA reductase inhibitors
Lovastatin (Mevacor, Altroprev Lipitor),
Simvastatin (Zocor) Atorvastatin
(Vytorin), Simvastatin-Ezetimibe (Zetia)
Calcium - Channel Blockers (Anti-hypertensives)
Felodipine (Plendil), Nifedipine (Adalat,
Procardia), Nimodipine (Nimotop),
Nicardipine (Cardene), Verapamil (Calan),
Amlodipine (Norvasc), Diltiazem (Cartia,
Cardizem), Nisoldipine (Sular),
Nitrendipine, Pranidipine.
Protease Inhibitors
Saquinavir (Invirase)
Warfarin
(Coumadin), (Jantoven)
Recommendations: If you are taking any of these drugs, remain consistent with
juice consumption until you consult your physician. Other fruits that may exhibit
the same interactions with these drugs include limejuice, Seville oranges and
tangelo juice. Let your physician know if you consume excessive amounts of
grapefruit juice and are presently taking any of these drugs.
Page 35 of 51

Page 36 of 51

Page 38 of 51
Social Services
The Social Services Department provides services within the vision of the Alomere
Health’s overall purpose and philosophy.
The Social Services Department focuses on the following purposes:
To provide services to all patients regardless of race, color, sex,
creed or ability to pay.
To ensure that services are provided with safety, dignity and privacy
to patients and their families.
To promote an awareness among the public of social services
availability to them at the hospital and through other health care
delivery units in the community and area.
Social Work is a very important part of the medical care. Illness can often be
precipitated, intensified and prolonged by problems in a person’s personal life and
environment. Unless these pressures in the personal life of the patient are either
prevented or relieved, they may slow down or even negate the effectiveness of the
medical treatments. It is essential, therefore, to have a service available to help
the patient modify these personal issues, which affect the patients’ health. If they
cannot be changed, the patient needs guidance and support in the acceptance or
endurance of them.
The Social Worker at Alomere Health functions as a member of the
multidisciplinary team which consists of physicians, nurses, physical, occupational
and speech therapy. Upon referral, the social worker assesses the patient’s and
family needs and formulates plans for their discharge. Social workers assist
patients with nursing home placements, arrangements for Home Health Services,
durable medical equipment, questions concerning financial resources, and Health
Care Directives.
Alomere Health Social Workers have a Bachelor’s Degree and
are licensed by the State of Minnesota.
For more information on Social Services at Alomere Health, call:
320-762-6108.
Page 39 of 51
If You are
60 Years or Older
The Senior LinkAge line has established
a service to assist you by providing a
“One Stop Shop for Minnesota
Seniors.”
This is in regards to housing options with
services, as well as other in-home
services to better assist you.
If you are interested, please contact the
Alomere Health Social Services before
your discharge.
After discharge, please call the Senior
Linkage at
1-800-333-2433

Page 40 of 51
Disclaimer:
The following pages that include lists of
resource options are for informational
purposes only - not all options are listed.
However, more contact information can
be obtained by contacting:
Alomere Health
Social Services Department.
320-762-6108
Page 41 of 51
Community Resources Information
Horizon Public Health:
Douglas, Grant, Pope, Stevens and Traverse Counties
320-763-6018
Todd County
320-732-4440
Social Services:
Douglas County Social Services
320-762-2302
Grant County Social Services
218-685-8200 or 1-800-291-2827
Ottertail County Social Services
218-998-8150
Pope County Social Services
320-634-5750
Stearns County Social Services
800-450-3663 or 320-656-6000
Stevens County Social Services
320-589-7400
Todd County Social Services
320-732-4500
Wadena County Social Services
218-631-7605
Parish Nurse Services:
First Lutheran Church, Ann Challes
320-762-2196
The Church of Saint Mary, Catholic Church, Vanessa Mensen
320-762-2320
Evangelical Covenant Church
320-762-1132
United Methodist Church
320-763-4624
Faith-Esther Lutheran Church (At this time they do not have one)
218-943-2891
St. Ann’s Catholic – Brandon or www.st[email protected]
(*No Parish Nurse but they have a list of people to assist their
members if needed)
320-834-5095
Senior Citizen Office, 806 Fillmore Street, Suite 1195,
Alexandria, MN 56308
320-762-3047
Senior Community Center, 414 Hawthorne Street, Alexandria
320-762-2087
Rainbow Rider and Senior Drivers
800-450-7770
Page 42 of 51
Senior Resources in Douglas County
For additional information or assistance
with referral to any of these resources,
contact Alomere Health Social Services at 762-6108
Home Delivered Meals: Nutritionally balanced meals delivered to the home. Contact
Senior Citizens' Office 320-762-3876.
Home Health Services: In-home care for persons needing assistance for medical
problems and daily living activities such as bathing, grooming, dressing or medication
reminders. Staff who provide care may include nurses, therapists, and/or home
health aides. See Home Health Services List.
Hospice: A special kind of care for dying people and their families that treats
physical, emotional, and spiritual needs. Contact Hospice of Douglas County 320-
763-6018 or Knute Hospice 320-759-1270 for Douglas County.
Homemaking/Housekeeping Services: Assistance with light housekeeping, such as
laundry, vacuuming, cleaning and meal preparation. See Home Health Services List.
Apartments Plus (Assisted Living): Private, apartment-style living with services
available as needed, including personal care assistance, meals, housekeeping,
activities, medication reminders, and 24-hour emergency response assistance. See
Services for a more detailed list.
Nursing Home: A licensed care facility offering 24-hour nursing services, meals,
personal care assistance, socialization, and programmed activities. Alexandria,
Bethany Nursing Home 320-762-1567 and Knute Nelson Nursing Home 320-763-
6653; Evansville—Evansville Care Campus 320-834-4466; Osakis, Galeon 320-859-
2142.
Senior Companion: This program helps homebound elderly remain independent by
helping them with medical appointments, groceries, errands, paper work, and by
being there to care. Senior Citizens' Office 320-762-3876.
Telephone Reassurance: Up to 24-hour telephone contact to reassure that, an
individual is safe. Volunteers and/or computers call at a preset time and alert others if
there is no answer. Senior Citizens' Office 320-762-3876. Bethany 320-763-2192,
Knute 320-759-1273, Heartland Security 888-264-6380
Care Call Plus: An emergency response phone that is monitored 24 hours a day. A
pendant activates the speakerphone from anywhere in your home when emergency
assistance is needed. Available to everyone.
Elder Network: A peer volunteer counseling service for elders (available to those 55
and older) by elders. A free in-home supportive service for individuals needing
emotional support due to life changes, loneliness, role changes, grieving, facing
difficult decisions, feelings of ongoing sadness, and other losses. Alexandria office
320-763-9084.
Fuel Assistance: (West Central Community Action Program) 320-762-3861 or
1-800-492-4805.
Page 43 of 51
Senior Resources - continued
Health Insurance Counseling Program: Free assistance with understanding and
interpreting insurance policies and Medicare given to seniors, age 60 and over, by
trained counselors. 320-762-3047.
Home Equipment Supplies: Such as oxygen, walkers, crutches, ostomy products,
elevated toilet seats, grab bars, walker replacement tips. See Medical Equipment List.
Support Groups: Cancer (Education Services of Alomere Health 320-762-6094);
Alzheimer’s (Minnesota Chapter 1-800-272-3900, First Lutheran 320-762-2196 Val
Trumm).
Page 44 of 51
Home Health Services and Local Nursing Homes
The attached listings are being provided for information purposes only. Some of
these agencies are public agencies and some are private agencies that have
requested to be placed on this list. Alomere Health is not affiliated with these
agencies and can provide no guarantees as to the quality or competency of their
service.
Home Health Services
Counties Served
Adara Home Health Inc.
330 Hwy 10 South
St. Cloud, MN 56304
Telephone:
320-255-1882 or 886-443-0092
Benton, Douglas, Morrison, Pope,
Sherburne, Stevens, Stearns, Todd,
Traverse, Wright.
Alliance Health Care
2204 East 117th Street
Burnsville, MN 55337
Telephone:
800-548-0980 or 320-214-7001(Willmar)
Douglas, Kandiyohi, Meeker, Pope,
Stearns, Stevens, Todd.
Aveanna Home Health
1600 Broadway
Alexandria, MN 56308
Telephone: 320-846-0002
St. Cloud Office
Telephone:
320-774-0777
Benton, Crow Wing, Douglas, Grant,
Kanabec, Kandiyohi, McCloud,
Meeker, Ottertail, Pope, Sherburne,
Stearns Todd, Traverse, Wright.
Barnabas Health Care Services, Inc.
223 Washington Street
Brainerd, MN 56401
Telephone:
218-829-0901 or 800-434-7225
Aitkin, Cass, Crow Wing, Todd.
CentraCare Health Home Care &
Hospice
2035 15
th
Street North
St. Cloud, MN 56303
Telephone:
320-259-9375
Benton, Douglas, Hennepin, Mille Lacs,
Meeker, Morrison, Pope, Sherburne,
Stearns, Swift, Todd, Wright.
Page 45 of 51
Home Health Services ~ continued
Home Health Services
Counties Served
Glacial Ridge Homecare
10 Fourth Avenue Southeast
Glenwood, MN 56334
Telephone:
320-634-4521
Douglas, Kandiyohi, Pope, Stearns,
Stevens, Swift, Todd.
Good Neighbor Home Health Care
14387 Edgewood Drive
Baxter, MN 56425
Telephone:
218-829-9238
Cass, Crow Wing.
Graceville Health Center Home Health
115 West Second Street,
Graceville, MN 56240-0157
Telephone:
320-748-8211
Big Stone, Stevens, Traverse.
Knute Nelson Home Health & Hospice
2715 Highway 29 South Suite 103
Alexandria, MN 56308
Telephone:
320-759-1273
Aitken, Becker, Benton, Big Stone,
Cass, Clearwater, Crow Wing,
Douglas, Grant, Hubbard, Mille Lacs,
Morrison, Otter Tail, Pope, Stearns,
Stevens, Swift, Todd, Traverse,
Wadena & Wilken.
Lakewood Staples Home Health
401 Prairie Avenue Northeast
Staples, MN 56479
Telephone:
218-894-8080
Crow Wing, Morrison, Todd, Wadena.
LB Homes Health
824 South Sheridan Street
Fergus Falls, MN 56537
Telephone:
218-998-1400
Clay, Douglas, Grant, Ottertail, Wilken.
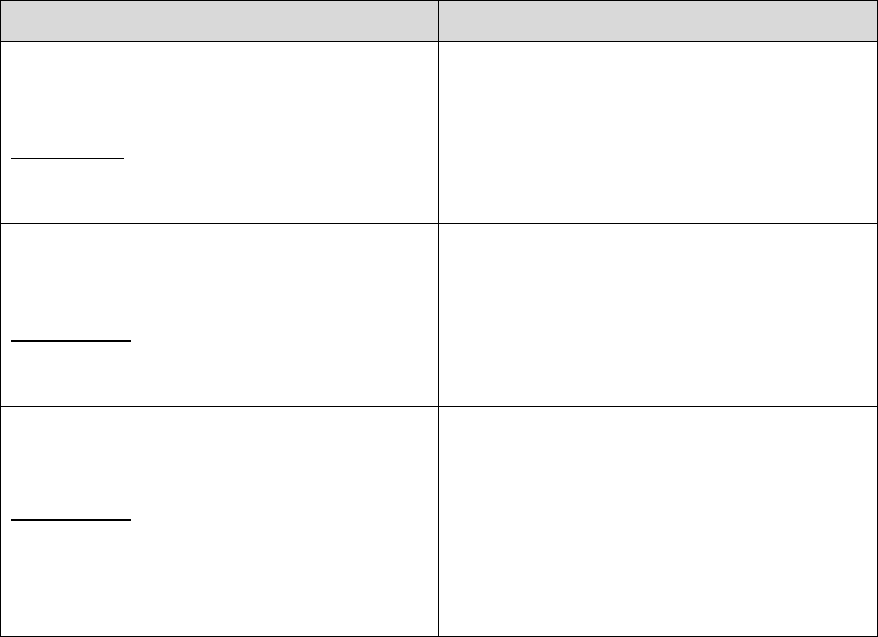
Page 46 of 51
Home Health Services ~ continued
Home Health Services
Counties Served
New Dimensions Home Health Care
PO Box 415,
Fergus Falls, MN 56537-0415
Telephone:
218-739-5856 or 800-395-9949
Becker, Big Stone, Douglas, Grant,
Itasca, Mahnomen, Ottertail, Pope,
Stevens, Traverse, Todd, Wilken.
Sanford Home Care
405 12
th
Street North
Wheaton, MN 56296
Telephone:
320-563-0078 or 320-695-2242
Big Stone, Grant, Stevens, Traverse.
Swift County - Benson Hospital
1815 Wisconsin Avenue
Benson, MN 56215
Telephone:
320-843-4232
or
320-843-1349 (Direct)
Chippewa, Kandiyohi, Pope, Swift.
Page 47 of 51
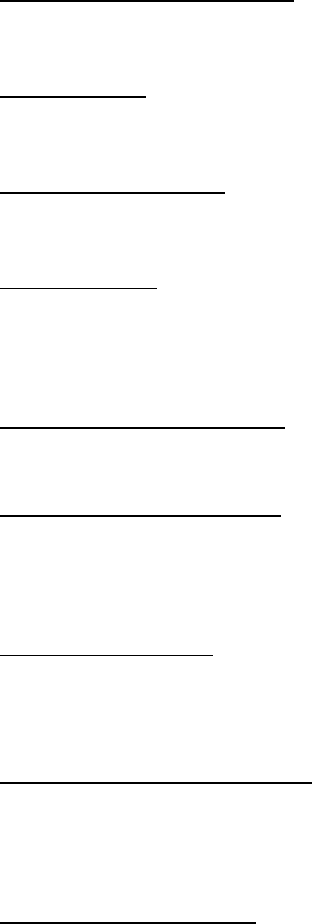
Local Nursing Homes
(Within 40 miles of Alexandria, MN)
Douglas County:
Knute Nelson Memorial Home: 420 – 12
th
Ave. East, Alexandria, 320-763-6653.
Skilled nursing facility. Medicare certified. Offers physical, occupational and speech
therapy.
Bethany Home: 1020 Lark St., Alexandria, 320-762-1567.
Skilled nursing facility. Medicare certified. Offers physical, occupational and speech
therapy.
Evansville Care Center: 649 State St, Evansville 320-834-4466 (26 miles).
Skilled nursing facility. Medicare certified. Offers physical, occupational and speech
therapy.
Galeon, Osakis: 410 West Main St., Osakis, 320-859-2142 (12 miles).
Skilled nursing facility. Medicare certified. Offers physical, occupational and speech
therapy. Assisted living/assisted living plus attached to nursing home.
Pope County:
Glenwood Retirement Village: 719 2
nd
St. S. E., Glenwood, 320-634-5131 (17
miles). Skilled nursing facility. Medicare certified. Offers physical, occupational and
speech therapy. Provides secure Alzheimer’s/dementia unit.
Minnewaska Lutheran Home: 605 North Main, Starbuck, 320-239-2217 (25 miles).
Skilled nursing facility. Medicare certified. Offers physical, occupational and speech
therapy.
Grant County:
Barrett Nursing Home: Hwy 55 & 59 South, Barrett, 320-528-2527 (30 miles).
Skilled nursing facility. Medicare certified. Offers physical, occupations and speech
therapy.
Stearns County:
CentraCare Health Sauk Centre: 425 Elm St., Sauk Centre, 320-351-1037 (29
miles). Skilled nursing facility. Medicare certified. Offer physical, occupational and
speech therapy.
Otter Tail County:
St. William’s Living Center: 212 W Soo St., Box 30, Parkers Prairie, 218-338-4671
(23 miles). Skilled nursing facility. Medicare certified. Offers physical, occupational
and speech therapy. Assisted living attached to nursing home.
***Miles Noted are Approximate from Alomere Health***
Page 48 of 51
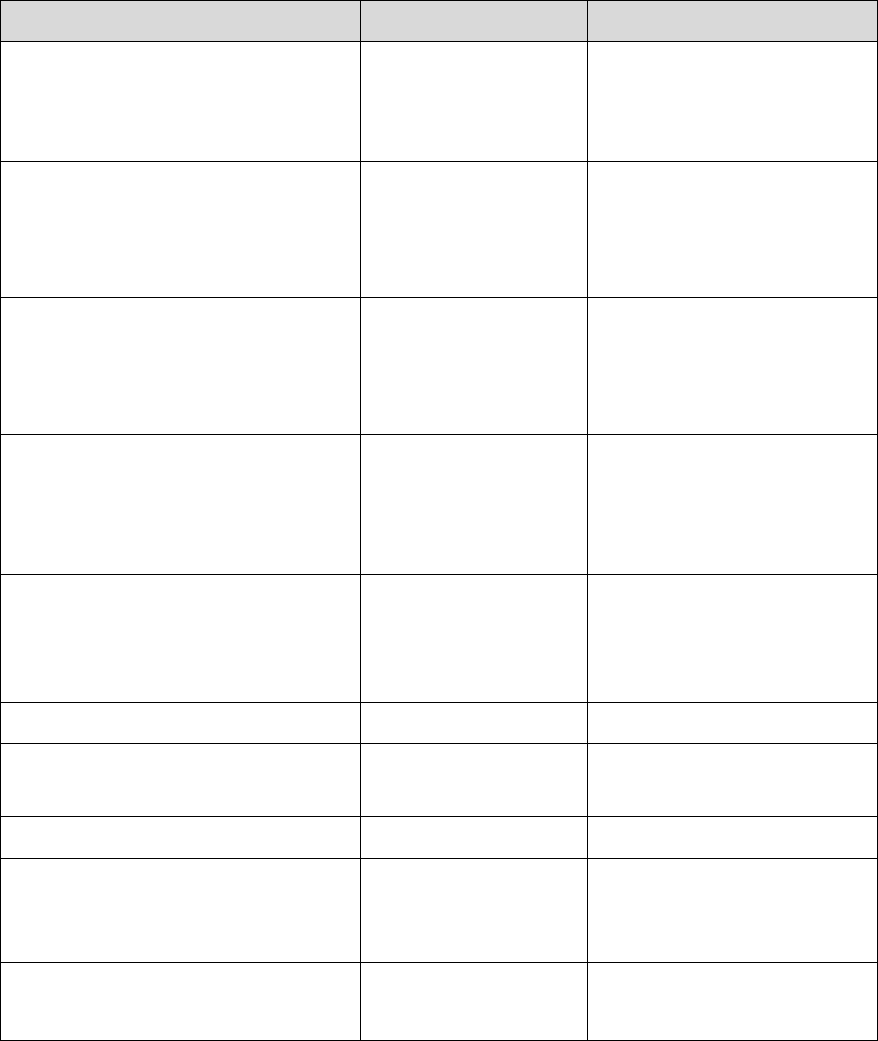
Local Hospice Providers
Organization
City
Phone
CentraCare Health Home
& Hospice
(Monday-Friday 8:00 am - 4:30 pm)
Sauk Centre
320-352-2221
320-351-1790
CHI Health at Home
Hospice
(Within 60 miles of Albany)
Albany
320-845-2440
Hospice of Douglas
County
(Within 30 miles of Alexandria)
Alexandria
320-763-6018
Glacial Ridge
(Pope, Douglas)
(Within 30 miles of Glenwood)
Glenwood
320-634-2221
866-667-4747
(toll free)
Knute Nelson Hospice
(Alexandria/Long Prairie/Morris/Elbow
Lake Offices)
Alexandria
320-759-1270
Moments Hospice
320-372-4380
Rice Hospice
Ortonville/Graceville
Ortonville
320-839-4124
Rice Hospice
Granite Falls
320-320-8217
Rice Hospice
Willmar
320-231-4450
800-336-7423
(toll free)
Rice Hospital
Benson
320-843-1308
Page 49 of 51
Medical Equipment / Medical Supplies
Home Equipment Providers
APRIA Healthcare
1501 Northway Drive
St. Cloud, MN 56303
(320) 252-0655
ProvidaCare Medical Supply
414 Great Oak Drive
Waite Park, MN 56387
(877) 557-7001
(320) 257-7001 (Fax)
Cornerstone Home Medical
225 Seventh Avenue East
Alexandria, MN 56308
(800) 637-7795
Sanford Health Equip
2633 Jefferson Street Suite 601
Alexandria, MN 56308
(320) 762-6858 or (218) 790-1481
LinCare
1650 College Way
Fergus Falls, MN 56537
(218) 739-4616 or (866)739-4616
Trumm Home Medical Specialties
610 Fillmore Street
Alexandria, MN 56308
(320) 763-2575 or (800) 272-7866
Medical Supplies
Lincare (Oxygen)
1650 College Way
Fergus Falls, MN 56537
(218)739-4616 IR (866)739-4616
(218)739-4616
Trumm Drug
600 Fillmore Street
Alexandria, MN 56308
(320) 763-3111
Target Pharmacy
4404 Hwy. 29 South
Alexandria, MN 56308
(320) 763-7393
Walgreens
Tenth and Broadway
Alexandria MN 56308
(320) 763-4360
Thrifty White Pharmacy
503 3
rd
Avenue East, Suite 100
Alexandria, MN 56308
(320) 762-1534
Walmart Pharmacy
515 50th Avenue West
Alexandria, MN 56308
(320) 762-2850
Page 50 of 51
Crisis Line / Local Mental Health &
Chemical Dependency Agencies
Crisis Line
Crisis Line/Suicide Information Line
1-800-784-2433
Region 4 Crisis Team Line
(Mental Health)
701-364-0431
Someplace Safe
(Shelter and safe housing advocacy for
domestic violence, sexual assault)
1-800-974-3359
Mental Health Agencies
Lakeland Mental Health Center
702 34
th
Avenue East
Alexandria, MN 56308
1-800-223-4512
320-762-2400
Lakeland Mental Health Center
100 17
th
Avenue NW, Suite 2
Glenwood, MN 56334
1-800-223-4512
320-634-3446
Lake Region Healthcare Bridgeway
712 Cascade Street South
Fergus Falls, MN 56537
1-218-736-8208
Lutheran Social Services
507 22
nd
Avenue East, Suite 1
Alexandria, MN 56308
1-320-762-5124
Chemical Dependency Agencies
Nystrom Substance Abuse Disorder
651-529-8479
Recovery Plus
(Address Chemical Dependency and
Mental Health Issues)
713 Anderson Avenue
St. Cloud, MN 56303
1-800-742-4357
Unity Recovery
320-219-7474
KH/lv/10-26-2023/Forms-2023/White Packet 2023 - 10-26-2023
Page 51 of 51
Patients and Family Members
If you are interested in reading some
scripture text during your stay, Bibles are
available.
Contact the Nursing Supervisor at 6139.
The Bibles are a gift from - The Gideons International